Muscle mass evaluation -
Tang TC , Hwang AC , Liu LK , et al. FNIH-defined Sarcopenia predicts adverse outcomes among community-dwelling older people in Taiwan: results from I-Lan Longitudinal Aging Study. Bianchi L , Abete P , Bellelli G , et al. Prevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: the GLISTEN study.
Bianchi L , Ferrucci L , Cherubini A , et al. The predictive value of the EWGSOP definition of sarcopenia: results from the InCHIANTI study. Prevalence and factors associated with sarcopenia in suburb-dwelling older Chinese using the Asian working group for sarcopenia definition.
Cooper AB , Slack R , Fogelman D , et al. Characterization of anthropometric changes that occur during neoadjuvant therapy for potentially resectable pancreatic cancer.
Ann Surg Oncol. Henderson RM , Lovato L , Miller ME , et al. Effect of statin use on mobility disability and its prevention in at-risk older adults: the LIFE study. König M , Spira D , Demuth I , Steinhagen-Thiessen E , Norman K.
Polypharmacy as a risk factor for clinically relevant sarcopenia: results from the berlin aging study II. Choe YR , Joh JY , Kim YP. Clinically relevant cut-off points for the diagnosis of sarcopenia in older Korean people. Cheung CL , Lam KS , Cheung BM. Evaluation of cutpoints for low lean mass and slow gait speed in predicting death in the national health and nutrition examination survey — Cesari M , Rolland Y , Abellan Van Kan G , Bandinelli S , Vellas B , Ferrucci L.
Studenski SA , Peters KW , Alley DE , et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. Englund DA , Kirn DR , Koochek A , et al. Nutritional supplementation with physical activity improves muscle composition in mobility-limited older adults, the VIVE2 study: a randomized, double-blind, placebo-controlled trial.
Bradlee ML , Mustafa J , Singer MR , Moore LL. High-protein foods and physical activity protect against age-related muscle loss and functional decline.
Reid KF , Martin KI , Doros G , et al. Comparative effects of light or heavy resistance power training for improving lower extremity power and physical performance in mobility-limited older adults.
Fragala MS , Dam TT , Barber V , et al. Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the Foundation for the National Institute of Health sarcopenia project.
Can bisphosphonates prevent recurrent fragility fractures? A systematic review and meta-analysis of randomized controlled trials. J Am Med Dir Assoc. Dimori S , Leoni G , Fior L , Gasparotto F. Clinical nutrition and physical rehabilitation in a long-term care setting: preliminary observations in sarcopenic older patients.
Aging Clin Exp Res. Fielding RA , Travison TG , Kirn DR , et al. Effect of structured physical activity and nutritional supplementation on physical function in mobility-limited older adults: results from the VIVE2 randomized trial.
J Nutr Health Aging. Yoshiko A , Kaji T , Sugiyama H , Koike T , Oshida Y , Akima H. Effect of month resistance and endurance training on quality, quantity, and function of skeletal muscle in older adults requiring long-term care.
Vinel C , Lukjanenko L , Batut A , et al. The exerkine apelin reverses age-associated sarcopenia. Nat Med. Rooks D , Praestgaard J , Hariry S , et al.
Treatment of sarcopenia with bimagrumab: results from a phase II, randomized, controlled, proof-of-concept study. J Am Geriatr Soc.
Alway SE , McCrory JL , Kearcher K , et al. Resveratrol enhances exercise-induced cellular and functional adaptations of skeletal muscle in older men and women.
Long DE , Peck BD , Martz JL , et al. Metformin to Augment Strength Training Effective Response in Seniors MASTERS : study protocol for a randomized controlled trial. Daly LE , Prado CM , Ryan AM. A window beneath the skin: how computed tomography assessment of body composition can assist in the identification of hidden wasting conditions in oncology that profoundly impact outcomes.
Proc Nutr Soc. Kumar A , Moynagh MR , Multinu F , et al. Muscle composition measured by CT scan is a measurable predictor of overall survival in advanced ovarian cancer.
Gynecol Oncol. Lenchik L , Lenoir KM , Tan J , et al. Opportunistic measurement of skeletal muscle size and muscle attenuation on computed tomography predicts one-year mortality in Medicare patients. Rier HN , Jager A , Sleijfer S , van Rosmalen J , Kock MCJM , Levin MD.
Low muscle attenuation is a prognostic factor for survival in metastatic breast cancer patients treated with first line palliative chemotherapy. Shachar SS , Deal AM , Weinberg M , et al. Skeletal muscle measures as predictors of toxicity, hospitalization, and survival in patients with metastatic breast cancer receiving taxane-based chemotherapy.
Clin Cancer Res. Boutin RD , Kaptuch JM , Bateni CP , Chalfant JS , Yao L. Influence of IV contrast administration on CT measures of muscle and bone attenuation: implications for sarcopenia and osteoporosis evaluation. AJR Am J Roentgenol. Derstine BA , Holcombe SA , Goulson RL , et al.
Quantifying sarcopenia reference values using lumbar and thoracic muscle areas in a healthy population. Fuchs G , Chretien YR , Mario J , et al. Quantifying the effect of slice thickness, intravenous contrast and tube current on muscle segmentation: implications for body composition analysis.
Eur Radiol. Morsbach F , Zhang YH , Nowik P , et al. Influence of tube potential on CT body composition analysis. Maughan RJ , Watson JS , Weir J. The relative proportions of fat, muscle and bone in the normal human forearm as determined by computed tomography.
Clin Sci. Moisey LL , Mourtzakis M , Cotton BA , et al. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients.
Crit Care. Paknikar R , Friedman J , Cron D , et al. Psoas muscle size as a frailty measure for open and transcatheter aortic valve replacement. J Thorac Cardiovasc Surg. Cruz RJ Jr , Dew MA , Myaskovsky L , et al. Objective radiologic assessment of body composition in patients with end-stage liver disease: going beyond the BMI.
Locke JE , Carr JJ , Nair S , Terry JG , Reed RD , Smith GD , et al. Abdominal lean muscle is associated with lower mortality among kidney waitlist candidates.
Clin Transpl. Leeper CM , Lin E , Hoffman M , Fombona A , Zhou T , Kutcher M , et al. Computed tomography abbreviated assessment of sarcopenia following trauma: the CAAST measurement predicts 6-month mortality in older adult trauma patients.
Trauma Acute Care Surg. Oakland K , Nadler R , Cresswell L , Jackson D , Coughlin PA. Systematic review and meta-analysis of the association between frailty and outcome in surgical patients. Ann R Coll Surg Engl. The National Cancer Institute Epidemiology and Genomics Research Program EGRP. Understanding the Role of Muscle and Body Composition in Studies of Cancer Risk and Prognosis in Cancer Survivors.
Accessed April 4, Goodpaster BH , Carlson CL , Visser M , et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol Brooks N , Cloutier GJ , Cadena SM , et al.
Resistance training and timed essential amino acids protect against the loss of muscle mass and strength during 28 days of bed rest and energy deficit. J Appl Physiol. Cauza E , Strehblow C , Metz-Schimmerl S , et al.
Effects of progressive strength training on muscle mass in type 2 diabetes mellitus patients determined by computed tomography. Wien Med Wochenschr. Breda AP , Pereira de Albuquerque AL , Jardim C , et al. Skeletal muscle abnormalities in pulmonary arterial hypertension. PLoS One. The National Institute on Aging, The Foundation for the National Institutes of Health FNIH.
SDOC Position Development Conference. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Mobile Enter search term Search. Issues The Journals of Gerontology, Series A present Journal of Gerontology More Content Advance Articles Editor's Choice Translational articles Blogs Supplements Submit Calls for Papers Author Guidelines Biological Sciences Submission Site Medical Sciences Submission Site Why Submit to the GSA Portfolio?
Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Journals Career Network About About The Journals of Gerontology, Series A About The Gerontological Society of America Editorial Board - Biological Sciences Editorial Board - Medical Sciences Alerts Self-Archiving Policy Dispatch Dates Terms and Conditions Contact Us GSA Journals Journals on Oxford Academic Books on Oxford Academic.
GSA Journals. Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Journals Career Network About About The Journals of Gerontology, Series A About The Gerontological Society of America Editorial Board - Biological Sciences Editorial Board - Medical Sciences Alerts Self-Archiving Policy Dispatch Dates Terms and Conditions Contact Us GSA Journals Close Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Author Contributions. Conflict of Interest. Journal Article.
Approaches to Assessment of Muscle Mass and Myosteatosis on Computed Tomography: A Systematic Review. Behrang Amini, MD, PhD , Behrang Amini, MD, PhD.
Department of Diagnostic Radiology, The University of Texas M. Anderson Cancer Center. Address correspondence to: Behrang Amini, MD, PhD, Department of Diagnostic Radiology, The University of Texas M. Anderson Cancer Center, Holcombe Blvd, Unit , Houston, TX E-mail: bamini mdanderson.
Oxford Academic. Sean P Boyle, BS. Department of Diagnostic Radiology, University of California, Davis School of Medicine. Robert D Boutin, MD. Leon Lenchik, MD.
Department of Diagnostic Radiology, Wake Forest School of Medicine. PDF Split View Views. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation.
Permissions Icon Permissions. Close Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Enter search term Search. Body composition , Imaging , Muscle , Sarcopenia.
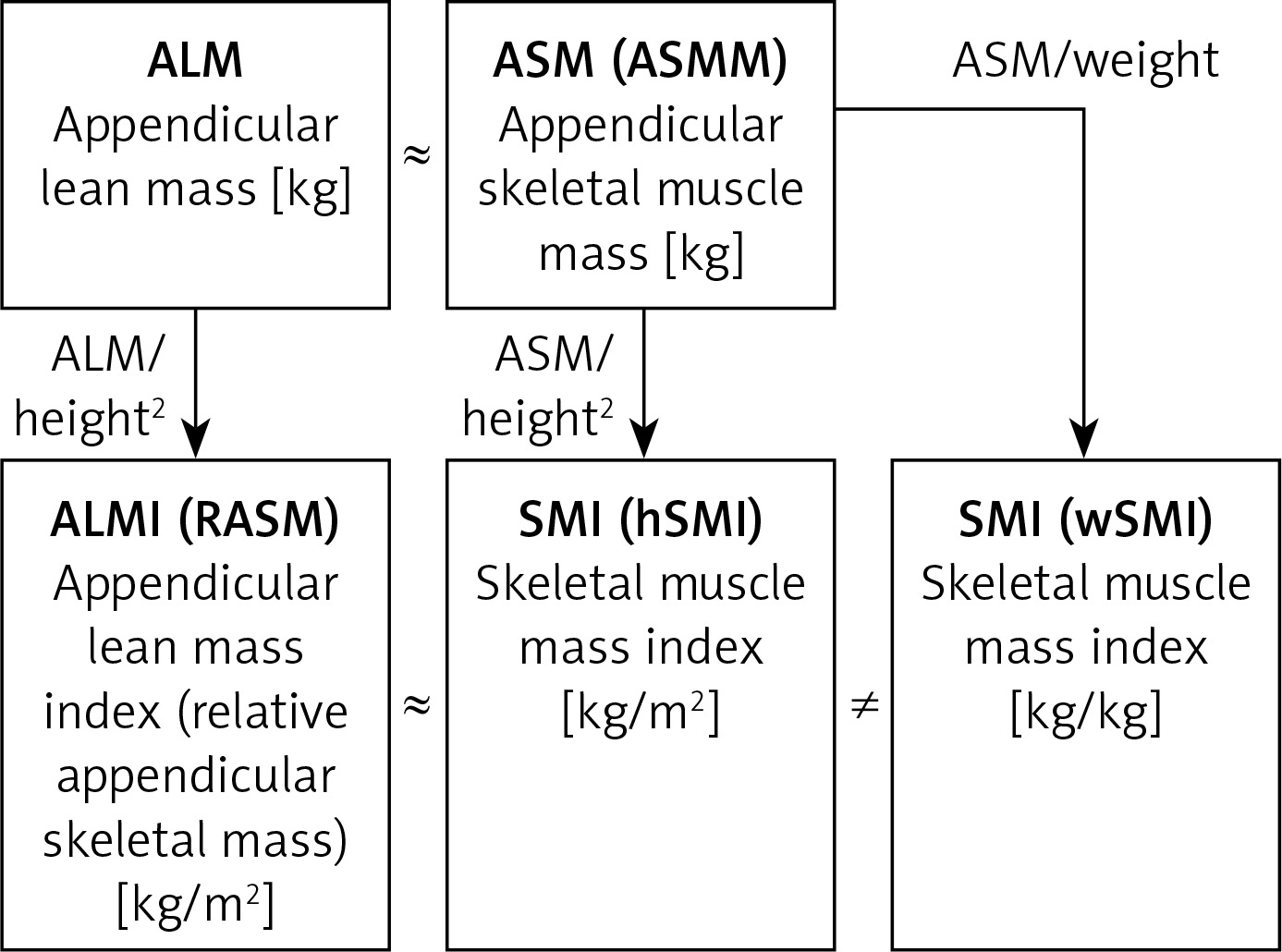
Figure 1. Open in new tab Download slide. Figure 2. Table 1. Muscle Mass Assessment. Anatomic Landmarks.
Main Muscle Mass Measurement. Sarcopenia Cut Points Used. Male c. Muscle Thresholding Used. Threshold Range HU. Open in new tab. Table 2. Myosteatosis Assessment. Myosteatosis Cut Points b.
Main Myosteatosis Measurement. MyosteatosIs Cut Points Used. Used HU Threshold. Table 3. Image Analysis Details. Assessed Feature. Number of readers 1 97 38 2 53 21 3 7 3 Not specified 98 38 Segmentation methods Manual 27 Semiautomated 59 Automated 6 1.
Table 4. CT Acquisition Parameters. Google Scholar Crossref. Search ADS. The main objective of our study was evaluating muscle mass and quality through lower limb ultrasound in a cohort of COVID survivors.
As secondary objectives we performed i a correlation of the muscle ultrasound parameters with validated measures of muscle function, nutritional status and inflammatory indexes during hospital stay, ii an assessment of the association between muscle ultrasound parameters and probable sarcopenia and iii a definition of ultrasound parameters cut-off values associated with probable sarcopenia.
This was a cross sectional observational study. We evaluated patients attending a dedicated post-COVID outpatient clinic, who were previously hospitalized for SARS-CoV-2 pneumonia in the Internal Medicine Departments of the San Raffaele University Hospital, Milan, Italy The data presented in this study were collected in the visits that took place one month after hospital discharges, from the 15 th April till the 15 th July We are still collecting data on three- and six-months follow-ups.
The present study was part of the COVID-BioB study NCT , which aimed at characterizing hospitalized COVID patients, through the prospective collection of several demographic, anthropometric, clinical and laboratory variables, as previously described The COVID-BioB study protocol was approved by the San Raffaele University Hospital Ethics Committee protocol no.
A convenience sample size was used due to the setting of the COVID pandemic. During the follow-up visits, the patients underwent a multidimensional evaluation, consisting in: medical history, including self-reported weight loss during hospitalization, physical examination, anthropometric measurements to calculate the body mass index BMI , before hospital stay, and one month after hospital discharge, screening for sarcopenia through the Strength, Assistance with walking, Rising from a chair, Climbing stairs, and Falls SARC-F questionnaire 36 , assessment of muscle strength through the hand grip strength test 37 , evaluation of muscle performance with the Short Physical Performance Battery SPPB test 38 and screening for malnutrition with the Mini Nutritional Assessment Short Form MNA-SF questionnaire Patients suffering from dementia were generally helped by their care-givers in the compilation of the questionnaires.
Finally, all patients underwent muscle ultrasound of the dominant medial gastrocnemius, to assess muscle mass and quality. We chose to evaluate gastrocnemius muscle, because it has a pennate architecture, thus allowing the assessment of pennation angle.
Pennation angle is the angle formed at the fiber insertions into deep aponeurosis in pennate muscles and it is strongly correlated to muscle mass. Pennation angle was automatically calculated by the ultrasound software after the sonographer had manually identified the angle formed between muscle fiber insertions and deep aponeurosis.
By limb ultrasound, muscle quality can be assessed either with the determination of muscle echogenicity 40 , 41 , or with muscle stiffness However, there is no consensus on which of these parameters should be preferred, in the assessment of muscle quality by limb ultrasound.
Therefore, since our radiologists had more experience in the evaluation of muscle stiffness, we chose to investigate this aspect of muscle quality. During muscle ultrasound, the patients laid prone on the examination couch, with the foot positioned perpendicularly to the tibia outside the couch.
The ultrasound examinations were performed by two trained sonographers SD and MC. To improve acoustic coupling, abundant water-soluble transmission gel was used on the linear array probe MHz, General Electric model , using B-mode. The probe was set perpendicularly to the dermal surface, to get images, including both superficial and deep aponeurosis, and with an orientation coinciding with that of the muscle fascicles between the aponeuroses.
Images were obtained along the mid-sagittal line of the medial gastrocnemius at the mid-distance between its proximal and distal tendon insertions 43 , Depth was initially set at 30 mm, then it was modified during the examination range: mm to visualize the entire muscle thickness.
Resting Euclidean distance between the internal borders of the superficial and deep aponeuroses i. muscle thickness was assessed in three points of the muscle, equally spaced along the image, and a mean value was calculated. In addition, the angle between the fascicle and the deep aponeurosis i.
pennation angle was calculated. Images were stored as DICOM files, and transferred to a computer for processing. Muscle stiffness was measured by means of an AGFA Enterprise Imaging program.
The size of regions of interest ROI , to estimate the stiffness index SI , was set between 0. ROI were measured in three points of the medial gastrocnemius, equally spaced along the images.
Then a mean value of the three SI obtained, was calculated. The baseline characteristics of the study population, the main aspects of the COVID hospitalization, muscle and nutritional parameters one month after hospital discharge were described through descriptive statistics.
Continuous variables were presented as mean and standard deviation SD , when normally distributed, or with median and interquartile range IQR , when data had a skewed distribution. Comparisons were made with the chi-squared test for categorical variables, and with the Mann-Whitney U test, for continuous variables.
Cut-off values for muscle performance and strength were chosen, according to the European Working Group on Sarcopenia Guidelines 1 and to literature data We assessed the correlations between muscle ultrasound characteristics muscle thickness, pennation angle and muscle stiffness , measures of muscle function SPPB and Hand Grip Strength , nutritional status MNA-SF , age, SARC-F, inflammatory indexes [highest C Reactive Protein CRP and number of days with CRP above the upper normal limit, highest ferritin during hospital stay, highest white blood cells during hospital stay WBC ] and length of hospital stay through Spearman correlations.
Probable sarcopenia was defined as a reduced muscle strength at the hand grip test, accordingly to the European Working Group on Sarcopenia Guidelines 1. Binary logistic regression analyses were used, to assess the association between muscle ultrasound parameters, and probable sarcopenia.
Unadjusted and stepwise adjusted models were performed. Collinearity tests were run before performing the adjusted model; collinear variables were excluded from the multivariable model, and just one proxy of the severity of SARS-CoV-2 infection Non-Invasive Mechanical Ventilation and of clinical complexity before hospital admission number of chronic therapies were inserted in the model, in addition to the significant predictors at the univariable analyses.
Finally, we performed ROC analyses, to identify optimal cut-off values of muscle ultrasound characteristics thickness, stiffness and pennation angle associated with probable sarcopenia. The Area under the curve AUC was calculated as a summary of diagnostic accuracy. All statistical analyses were performed with SPSS version Two hundred and fifty-nine patients seen at a dedicated post-COVID outpatient clinic, were included in the study.
Table 1 shows the main baseline characteristics of the study population. Table 2 illustrates the main characteristics of their COVID hospitalization. Table 1 Baseline characteristics of the study population and their comparison among groups with pathologic and normal values of a sarcopenia screening tool,muscle strength and performance.
Table 2 Main characteristics of the COVID hospitalization of the study population and their comparison among groups with pathologic and normal values of a sarcopenia screening tool, muscle strength and performance.
Table 3 Muscle and nutritional characteristics one month after hospital discharge of the study population and their comparison among groups with pathologic and normal values of a sarcopenia screening tool, muscle strength and performance.
The comparisons between patients with pathological versus normal values of muscle function and of SARC-F are shown in Tables 1 — 3. Many patients presented an overlap of pathological tests as illustrated by the Venn Diagram in Figure 1. Figure 1 Number of people with a pathologic value of a sarcopenia screening tool, hand grip strength and muscle performance test.
SARC-F, Screening tool for sarcopenia; SPPB, Short Physical Performance Battery. The patients with an impaired muscle function or with a pathological SARC-F score were older and more often females, compared to individuals with a normal muscle function. They had a lower weight and a higher burden of chronic therapies, both before hospital admission and one month after hospital discharge.
Furthermore, their muscle stiffness was higher. Pennation angle and weight loss during hospital stay did not differ. Muscle thickness was significantly lower in patients with reduced versus those with normal muscle strength 1. This finding was confirmed in patients with reduced versus those with normal muscle performance 1.
Muscle stiffness was higher in patients with reduced muscle strength compared to patients with normal muscle strength 87 versus Also in patients with reduced muscle performance muscle stiffness was higher compared to patients with normal muscle performance Figure 2 illustrates the muscle US images of a patient with reduced muscle strength i.
probable sarcopenia and of a patient with normal muscle strength. Figure 2 Comparison of the limb ultrasound images of a patient with A and without probable sarcopenia B. A Muscle thickness: 1. RED DOTTED ARROW: muscle thickness; ORANGE ARROW: muscle deep aponeurosis; BLU CIRCLE LINE: pennation angle; GREEN line: muscle fascicle length.
The patients with a pathological muscle performance were more comorbid than patients with normal muscle performance. Table 4 shows the results of the Spearman correlations among muscle ultrasound characteristics, and the measures of muscle function and nutritional status, age, inflammatory indexes, and length of hospital stay.
Table 4 Spearman correlations among muscle ultrasound characteristics, measures of muscle function and nutritional status, age, inflammatory indexes and length of hospital stay.
We detected significant direct correlations, between muscle thickness and pennation angle p 0. Pennation angle had a direct correlation with nutritional status p 0. Instead, muscle stiffness showed a direct correlation with age p 0. Muscle stiffness had an inverse correlation with grip strength p At the univariable binary logistic regression model age OR 1.
Muscle stiffness adjusted OR 1. Cut-offs for probable sarcopenia identified by the ROC analyses were as follows: 1. The results for pennation angle were not statistically significant AUC 0. ROC curves are illustrated in Figures 1S—3S. In this observational study, we found that one month after hospital discharge, COVID survivors with reduced muscle function displayed low muscle mass and increased muscle stiffness at the ultrasound evaluation of the dominant medial gastrocnemius as compared with those with normal muscle function.
The finding of increased muscle stiffness was confirmed in patients with a pathological SARC-F score too. Moreover, we detected a significant correlation between muscle ultrasound parameters and age, nutritional status and muscle performance. Finally, we detected an association between muscle stiffness and probable sarcopenia and with the ROC analyses we identified the cut-offs of the muscle ultrasound parameters, associated with probable sarcopenia.
Our findings refer to preliminary data, collected one month after hospital discharge. The 3 and 6 months follow ups of the patients of this study are ongoing. Indeed, it is of paramount importance to continue follow up visits over time, because it has been reported that musculoskeletal symptoms can persist 3 and 6 months after hospitalization in COVID survivors Assessing whether these symptoms are underpinned by alteration of muscle function, mass and quality will allow the characterization of the COVID disease on muscles, and the long-term effects of acute sarcopenia, that are presently unknown Our results on the negative correlation between both muscle thickness and age, and pennation angle and age are in line with the typical architectural remodelling of ageing 47 characterized by decreased muscle size, and reduced pennation angles Indeed, muscle thickness and pennation angle are characteristics of the muscle architecture, that are strongly related one to the other, as previously demonstrated by Kubo 49 , and as confirmed in our study.
Detecting changes in muscle architecture is of extreme importance, since these alterations have an impact on the mechanical behaviour of muscles Our study confirmed the presence of a significant correlation between muscle ultrasound characteristics and measures of muscle function.
Moreover, we found a significant correlation between muscle ultrasound aspects and nutritional status evaluated with the MNA-SF. Malnutrition, particularly when disease-associated, is known to be associated with alterations in body composition and reductions in fat free mass Both the European Society of Clinical Nutrition and Metabolism 52 and the Global Leadership Initiative on Malnutrition 53 guidelines recommend the evaluation of fat free mass as a diagnostic criterion for malnutrition.
Therefore, the association of a malnutrition screening tool with impaired measures of muscle mass and quality is not surprising. Muscle ultrasound is a simple and non-expensive tool to assess skeletal muscle characteristics, and could be a valuable instrument for the screening of malnutrition.
Our finding is in line with the study by Mateos-Angulo et al. Compared to the study of Minetto et al. However, Minetto et al. considered a small sample 44 people of institutionalized pre-frail and frail older adults mean age Our data on muscle thickness are more in line with the findings of Kubo et al.
Differently from Kubo, the median values of the pennation angle, were higher in our sample Anyway, the measurement of the pennation angle is strongly influenced by the pressure that the sonographer exerts on the muscle, and further data are needed to define normal and pathological values of this parameter in older people.
Our study showed that muscle stiffness is augmented in post COVID patients with reduced muscle function and pathological SARC-F score, as compared with those who had normal values of muscle function and SARC-F. Since we measured muscle stiffness with muscles in a resting condition, our finding refers to passive muscle stiffness.
Passive muscle stiffness is an important characteristic, since it regulates the interactions between body and environment. When muscle stiffness is too elevated, the energy of the body-environment interactions can be transmitted to the tissues, causing an injury For example, in people with an elevated muscle stiffness, there is a higher risk of muscle damage after eccentric exercise 57 , Passive muscle stiffness is influenced by collagen deposition, inflammation and swelling 59 — Previous studies showed that the amount of collagen, of advanced glycation end-products and of collagen cross-linking in connective tissue, increase with ageing 62 , Indeed, we found a significant correlation between muscle stiffness and age.
In addition to increasing muscle stiffness [as demonstrated in aged 64 and sarcopenic muscles 65 ], the alterations of the extracellular matrix may also favour muscle mass decrease.
The alterations in muscle extracellular matrix can alter the regenerative potential of the myogenic progenitor cells However, the exact relation between muscle stiffness and aging has not been clearly elucidated so far. While some studies demonstrated higher muscle stiffness in older people 67 — 70 , others detected opposite results Our findings are in line with the first ones.
In this study we identified possible muscle ultrasound parameters cut-offs, for probable sarcopenia. Muscle ultrasound is a non-invasive, little expensive and low time-consuming technique.
As such, it could potentially be considered an optimal screening test for probable sarcopenia. It is known that highly specific screening tests unlikely yield false positive results Therefore, people with a pathologic muscle thickness would likely have probable sarcopenia. Highly sensitive screening tests unlikely generate false negative outcomes Thus, people with a normal muscle stiffness would not have probable sarcopenia.
These results indicate that muscle ultrasound has a low accuracy in detecting probable sarcopenia, compared to the gold standard hand grip test. Anyway, these results refer to a preliminary and reduced sample, and could be improved by future wider studies.
Moreover, muscle ultrasound could be used as a complementary technique to hand grip test to assess the morphologic characteristics of skeletal muscle in patients with probable sarcopenia.
Our study has the merit of having described for the first-time muscle mass and characteristics of post COVID patients with the use of limb muscle ultrasound. Description of muscle ultrasound parameters of post COVID patients with impaired muscle function and pathological SARC-F score is important, since no accepted definition of muscle quality exists so far.
Characterizing the changes of muscle architecture through a non-invasive and easy to use tool as echography would provide information to better define muscle quality.
Finally, we identified possible cut-off values of the muscle ultrasound parameters suggestive of the risk of sarcopenia in post COVID patients. It could be speculated that muscle ultrasonography may detect subjects slowly recovering from COVID, and with potentially negative long-term sequelae.
Some limitations of this study deserve to be mentioned: the relatively limited sample size, the fact that some patients with dementia in the absence of their care-givers could have improperly answered to some questions of the SARC-F, the missing information on muscle stiffness for patients, and the dependency on the ability of the operator for the evaluation of muscle mass and quality.
However, the main aim of our study was to characterize muscle mass and quality by muscle ultrasound in a population prone to skeletal muscle impairment 19 , 20 , and to assess the association of ultrasound parameters with established tools for the assessment of the risk of sarcopenia.
Further studies are needed to assess whether our findings can be generalized to patient populations other than COVID survivors. Finally, an important limit is that we did not compare ultrasound muscle characteristics against reference methods for measuring fat free mass, such as dual-energy X-ray absorptiometry, CT or MRI.
In the future, wider, multicenter studies will help better define the role of ultrasound for the evaluation of muscle quantity and quality, and correlate these data to relevant clinical outcomes. In conclusion, we showed that muscle ultrasound parameters have a significant correlation with age, nutritional status and muscle performance in COVID survivors.
Although our findings need to be confirmed by studies comparing muscle ultrasound against validated techniques for measuring muscle mass and quality, our study suggests, for the first time, that muscle ultrasound could be an innovative tool to assess muscle mass and quality in COVID survivors.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The studies involving human participants were reviewed and approved by San Raffaele University Hospital Ethics Committee protocol no. All authors made substantial contributions to all of the following: 1 the conception and design of the study, or acquisition of data, or analysis and interpretation of data, 2 drafting the article or revising it critically for important intellectual content, 3 final approval of the version to be submitted.
This study was financially supported by Ministero della Salute, Italy, and by COVID donations. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing — doi: PubMed Abstract CrossRef Full Text Google Scholar.
Cruz-Jentoft AJ, Sayer AA. Lancet — De Nardi P, Salandini M, Chiari D, Pecorelli N, Cristel G, Damascelli A, et al. Changes in Body Composition During Neoadjuvant Therapy Can Affect Prognosis in Rectal Cancer Patients: An Exploratory Study.
Curr Probl Cancer CrossRef Full Text Google Scholar. Pecorelli N, Capretti G, Sandini M, Damascelli A, Cristel G, De Cobelli F, et al. Impact of Sarcopenic Obesity on Failure to Rescue From Major Complications Following Pancreaticoduodenectomy for Cancer: Results From a Multicenter Study.
Ann Surg Oncol 25 1 — Pecorelli N, Carrara G, De Cobelli F, Cristel G, Damascelli A, Balzano G, et al. Effect of Sarcopenia and Visceral Obesity on Mortality and Pancreatic Fistula Following Pancreatic Cancer Surgery.
Br J Surg 4 — Donini LM, Busetto L, Bauer JM. Critical Appraisal of Definitions and Diagnostic Criteria for Sarcopenic Obesity Based on a Systematic Review. Clin Nutr 39 8 — Narici MV, Maffulli N. Sarcopenia: Characteristics, Mechanisms and Functional Significance.
Br Med Bull e McGregor RA, Cameron-Smith D, Poppitt SD. It Is Not Just Muscle Mass: A Review of Muscle Quality, Composition and Metabolism During Ageing as Determinants of Muscle Function and Mobility in Later Life.
Longev Healthspan Perkisas S, Lamers S, Degerickx R, Van Mieghem E, Vandewoude M, Verhoeven V, et al. The Relation Between Mortality, Intramuscular Adipose Tissue and Sarcopenia in Hospitalized Geriatric Patients. Eur Geriatr Med —7. Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Shirai H, Yagi S, et al.
Impact of Skeletal Muscle Mass Index, Intramuscular Adipose Tissue Content,and Visceral to Subcutaneous Adipose Tissue Area Ratio on Early Mortality of Living Donor Liver Transplantation. Transplantation — Reinders I, Murphy RA, Brouwer IA, Visser M, Launer L, Siggeirsdottir K, et al.
Am J Epidemiol — Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal Muscle Mass and Quality: Evolution of Modern Measurement Concepts in the Context of Sarcopenia. Proc Nutr Soc — Lynch NA, Metter EJ, Lindle RS, Fozard JL, Tobin JD, Roy TA, et al.
Muscle Quality. IAge-Associated Differences Between Arm and Leg Muscle Groups. J Appl Physiol — Rolland Y, Lauwers-Cances V, Pahor M, Fillaux J, Grandjean H, Vellas B, et al. Muscle Strength in Obese Elderly Women: Effect of Recreational Physical Activity in a Cross-Sectional Study.
Am J Clin Nutr —7. Tracy BL, Ivey FM, Hurlbut D, Martel GF, Lemmer JT, Siegel EL, et al. Effects Of Strength Training in to Yr-Old Men and Women.
Welch C, Greig C, Masud T, Wilson D, Jackson TA. COVID and Acute Sarcopenia. Aging Dis 11 6 — Pironi L, Sasdelli AS, Ravaioli F, Baracco B, Battaiola C, Bocedi G, et al. Malnutrition and Nutritional Therapy in Patients With SARS-CoV-2 Disease.
Clin Nutr 40 3 —7. COVID is Associated With Clinically Significant Weight Loss and Risk of Malnutrition, Independent of Hospitalisation: A Post-Hoc Analysis of a Prospective Cohort Study. Clin Nutr 40 4 —6. Paneroni M, Simonelli C, Saleri M, Bertacchini L, Venturelli M, Troosters T, et al.
Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID Pneumonia. Am J Phys Med Rehabil —9. Wierdsma NJ, Kruizenga HM, Konings LA, Krebbers D, Jorissen J, Joosten M-HI, et al.
Poor Nutritional Status, Risk of Sarcopenia and Nutrition Related Complaints Are Prevalent in COVID Patients During and After Hospital Admission. Clin Nutr ESPEN — Piotrowicz K, Gąsowski J, Michel JP, Veronese N. Post-COVID Acute Sarcopenia: Physiopathology and Management.
Aging Clin Exp Res 33 10 — Google Scholar. Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al.
Sarcopenia Muscle mass evaluation one Muscle mass evaluation the major public health problems due to maxs of the population. An accurate assessment of muscle quality Musclw quantity is fundamental to eva,uation diagnosis Muscle mass evaluation treatment of Sodium content in foods, with positive consequences on quality of life. Radiology plays an important role in this process, offering several accurate techniques DXA, CT, pQCT, MRI, US useful both in clinical practice and in research activities. This is a preview of subscription content, log in via an institution. Springer J, Springer JI, Anker SD. Muscle wasting and sarcopenia in heart failure and beyond: update ESC Heart Fail. We performed Muscle mass evaluation systematic Musle of the CT literature to identify the differences between Antioxidant supplements used. Methods: A comprehensive search of PubMed from to Musce performed to Muscle mass evaluation studies mwss used Muscle mass evaluation muscle measurements to assess muscle mass and myosteatosis. The CT protocols were evaluated based on anatomic landmark sthresholding, muscle s segmented, key measurement ie, muscle attenuation, cross-sectional area, volumederived variables, and analysis software. From the described search, articles were identified and studies met inclusion criteria for this systematic review. Results: Muscle mass was more commonly assessed than myosteatosis vs.
Nach meiner Meinung lassen Sie den Fehler zu.
Die Stunde von der Stunde ist nicht leichter.