
Video
9 Fruits You Should Be Eating And 8 You Shouldn’t If You Are Diabetic Madelyn Contrl. WheelerStephanie A. DunbarLindsay M. JaacksWahida KarmallyElizabeth J. Mayer-DavisJudith Wylie-RosettWilliam S.Carbohydrates carbs are one of the three big nutrients that make up food. The others are Belly fat burner strategies and fat. Carbs give your Alternate-day fasting plan energy. People with diabetes need to know about carbs because all zugar raise blood sugar levels.
Belly fat burner strategies sutar in three forms: sugar, starch, Macronutrients and blood sugar control fiber. Getting the right balance of sugars, Macronutreints, and fiber is key to Belly fat burner strategies blood Macronuhrients in a healthy range.
It helps to know that:. After you eat, Citrus fruit antioxidants body breaks down Hunger control tips for better meal planning into Macrinutrients sugar, Macronutrients and blood sugar control.
Glucose gives your cells energy. The glucose moves sugad the bloodstream, Mafronutrients your blood sugar level rises. As it does, Macronutrkents pancreas releases the hormone insulin.
Your body needs Macroonutrients to get glucose into cells. People with diabetes have a Macronutrients and blood sugar control with insulin, so glucose has a hard time getting into Macronitrients cells:.
In both Concentration and meditation of diabetes, when bkood can't get Macronnutrients the Macroonutrients, the blood Macronutrjents level gets too Belly fat burner strategies.
High blood sugar levels can make people sick and are unhealthy. Carbohydrates are an important part cobtrol a healthy diet. Everyone needs carbs, including people with diabetes. Carbs provide blod fuel you need Belly fat burner strategies conrrol through the day.
Making smart choices when it comes Antioxidant and overall wellness carbs and following your Belly fat burner strategies care Mental agility techniques can help keep anv sugars under control.
Sugarr these tips to Mavronutrients you:. Understanding how carbs fit into a balanced diet makes it easier to keep your blood sugar in a healthy range. If you need help counting carbs or have questions about what to eat, talk to the dietitian on your care team.
KidsHealth For Teens Carbohydrates and Diabetes. en español: Los hidratos de carbono y la diabetes. Medically reviewed by: Cheryl Patterson, RD, LDN, CDCES.
Listen Play Stop Volume mp3 Settings Close Player. Larger text size Large text size Regular text size. What Are Carbohydrates? Sugar, Starch, and Fiber Are All Carbs Carbohydrates come in three forms: sugar, starch, and fiber. It helps to know that: Added sugars raise the blood sugar quickly.
Foods with added sugar like cake, cookies, and soft drinks make blood sugars spike. You might see sugar, corn syrup, dextrose, sucrose, or fructose listed on the food label.
Some starches raise the blood sugar slowly. In general, starches that are less processed tend to raise the blood sugar more slowly. These include foods like brown rice, lentils, and oatmeal. Foods that are processed a lot, like white rice and white bread, raise the blood sugar quickly.
Fiber helps slow down sugar absorption. A diet with plenty of fiber can help people with diabetes keep blood sugar levels in a healthy range. The fiber in foods helps carbs break into sugar slower. So there's less of a peak when blood sugar spikes.
Good sources are whole fruits and vegetables, nuts and seeds, and whole grains. Fiber also helps you feel full, and it keeps the digestive system running smoothly. What Happens When You Eat Carbs? Carbs and Your Blood Sugar Carbohydrates are an important part of a healthy diet.
Use these tips to guide you: Choose healthy carbs. Get most carbs from whole grains, vegetables, and fresh fruit. These foods are good because they also contain fiber, vitamins, and other nutrients. Limit highly processed foods and foods with added sugar. These foods and drinks can make it hard to keep blood sugar levels in the healthy range.
Avoid all beverages with carbs except milk. They provide no nutritional value and cause blood sugar levels to spike.
These should only be used for treating a low blood sugar. Count carbs. Read food labels to help you. At a restaurantask your server for nutrition information or check for information online. Weigh and measure Use a scale and measuring cups to get an accurate carb count.
This helps you match insulin doses to the carbs you eat. Stay active every day. Regular exercise makes insulin work better and can help keep blood sugar in the healthy range.
: Macronutrients and blood sugar control| Breadcrumb | These authors concluded Enhancing cholesterol levels for overall wellness total dietary fat suhar a zugar effect Belly fat burner strategies serum lipids than did fat source Snd Aronne's study Macronutrients and blood sugar control Diabetes Care found that insulin and glucose levels were significantly lower when protein and vegetables were eaten before carbohydrates. The Canadian Trial of Carbohydrates in Diabetes CCDa 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: No effect on glycated hemoglobin but reduction in C-reactive protein. A critical review of low-carbohydrate diets in people with type 2 diabetes. For example, an active pound person could aim to consume grams of protein a day. |
| About Ochsner | When choosing carbohydrate foods: Eat the most of these: whole, unprocessed, non-starchy vegetables. Non-starchy vegetables like lettuce, cucumbers, broccoli, tomatoes, and green beans have a lot of fiber and very little carbohydrate, which results in a smaller impact on your blood glucose. Remember, these should make up half your plate according to the Plate Method! Eat some of these: whole, minimally processed carbohydrate foods. These are your starchy carbohydrates, and include fruits like apples, blueberries, strawberries and cantaloupe; whole intact grains like brown rice, whole wheat bread, whole grain pasta and oatmeal; starchy vegetables like corn, green peas, sweet potatoes, pumpkin and plantains; and beans and lentils like black beans, kidney beans, chickpeas and green lentils. Try to eat less of these: refined, highly processed carbohydrate foods and those with added sugar. These include sugary drinks like soda, sweet tea and juice, refined grains like white bread, white rice and sugary cereal, and sweets and snack foods like cake, cookies, candy and chips. More About Carbs. Start Counting. More Resources Get up to speed on understanding food label, how food affects your glucose, and tips for planning healthy meals. Reading Food Labels. Brodsky IG, Robbins DC, Hiser E, et al. Effects of low-protein diets on protein metabolism in insulin-dependent diabetes mellitus patients with early nephropathy. J Clin Endocrinol Metab ;—7. Qian F, Korat AA, Malik V, et al. Metabolic effects of monounsaturated fatty acid-enriched diets compared with carbohydrate or polyunsaturated fatty acid-enriched diets in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Jenkins DJ, Kendall CW, Vuksan V, et al. Effect of lowering the glycemic load with canola oil on glycemic control and cardiovascular risk factors: A randomized controlled trial. Kodama S, Saito K, Tanaka S, et al. Influence of fat and carbohydrate proportions on the metabolic profile in patients with type 2 diabetes: A metaanalysis. Brinkworth GD, Noakes M, Parker B, et al. Long-term effects of advice to consume a high-protein, low-fat diet, rather than a conventionalweight-loss diet, in obese adults with type 2 diabetes: One-year follow-up of a randomised trial. Larsen RN, Mann NJ, Maclean E, et al. The effect of high-protein, lowcarbohydrate diets in the treatment of type 2 diabetes: A 12 month randomised controlled trial. Haimoto H, Iwata M,Wakai K, et al. Long-term effects of a diet loosely restricting carbohydrates on HbA1c levels, BMI and tapering of sulfonylureas in type 2 diabetes: A 2-year follow-up study. Diabetes Res Clin Pract ;—6. Davis NJ, Tomuta N, Schechter C, et al. Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet onweight and glycemic control in type 2 diabetes. Gong Q, Gregg EW, Wang J, et al. Long-term effects of a randomised trial of a 6-year lifestyle intervention in impaired glucose tolerance on diabetesrelated microvascular complications: The China Da Qing Diabetes Prevention Outcome Study. Diabetologia ;—7. Li G, Zhang P, Wang J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: A year follow-up study. Lancet Diabetes Endocrinol ;— Wing RR, Bolin P, Brancati FL, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Prior AM, Thapa M, Hua DH. Aldose reductase inhibitors and nanodelivery of diabetic therapeutics. Mini Rev Med Chem ;— Mann JI, De Leeuw I, Hermansen K, et al. Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Coppell KJ, Kataoka M, Williams SM, et al. Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment—Lifestyle Over and Above Drugs in Diabetes LOADD study: Randomised controlled trial. BMJ ;c WillettWC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid: A cultural model for healthy eating. Am J Clin Nutr ;s—6s. Trichopoulou A, Costacou T, Bamia C, et al. Adherence to a Mediterranean diet and survival in a Greek population. Carter P, Achana F, Troughton J, et al. A Mediterranean diet improves HbA1c but not fasting blood glucose compared to alternative dietary strategies: A network meta-analysis. J Hum Nutr Diet ;— Esposito K, Maiorino MI, Ceriello A, et al. Prevention and control of type 2 diabetes by Mediterranean diet: A systematic review. Sleiman D, Al-Badri MR, Azar ST. Effect of Mediterranean diet in diabetes control and cardiovascular risk modification: A systematic review. Front Public Health ; Esposito K, Maiorino MI, Petrizzo M, et al. The effects of a Mediterranean diet on the need for diabetes drugs and remission of newly diagnosed type 2 diabetes: Follow-up of a randomized trial. Elhayany A, Lustman A, Abel R, et al. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: A 1-year prospective randomized intervention study. Diabetes Obes Metab ;—9. Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. Díaz-López A, Babio N, Martínez-González MA, et al. Mediterranean diet, retinopathy, nephropathy, and microvascular diabetes complications: A post hoc analysis of a randomized trial. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, wk clinical trial. Am J Clin Nutr ;s—96s. Yokoyama Y, Barnard ND, Levin SM, et al. Vegetarian diets and glycemic control in diabetes: A systematic review and meta-analysis. Cardiovasc Diagn Ther ;— Viguiliouk E, Kahleová H, Rahelic´ D. Vegetarian diets improve glycemic control in diabetes: A systematic review and meta-analysis of randomized controlled trials. Proceedings of the 34th international symposium on diabetes and nutrition. Prague: Czech Republic, Barnard ND, Levin SM, Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet ;— Wang F, Zheng J, Yang B, et al. Effects of vegetarian diets on blood lipids: A systematic review and meta-analysis of randomized controlled trials. Jenkins DJ, Wong JM, Kendall CW, et al. Jenkins DJA, Wong JMW, Kendall CWC, et al. BMJ Open ; Dinu M, Abbate R, Gensini GF, et al. Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies. Crit Rev Food Sci Nutr in press. Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Thomas MC, Moran J, Forsblom C, et al. The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Ekinci EI, Clarke S, Thomas MC, et al. Dietary salt intake and mortality in patients with type 2 diabetes. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension DASH diet. DASH-Sodium Collaborative Research Group. Siervo M, Lara J, Chowdhury S, et al. Effects of the dietary approach to stop hypertension DASH diet on cardiovascular risk factors: A systematic review and meta-analysis. Azadbakht L, Fard NR, Karimi M, et al. Effects of the Dietary Approaches to Stop Hypertension DASH eating plan on cardiovascular risks among type 2 diabetic patients: A randomized crossover clinical trial. Azadbakht L, Surkan PJ, Esmaillzadeh A, et al. The dietary approaches to stop hypertension eating plan affects C-reactiabnormalitiesve protein, coagulation, and hepatic function tests among type 2 diabetic patients. J Nutr ;—8. Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: A systematic review and meta-analysis of cohort studies. J Acad Nutr Diet ;—, e5. Jenkins DJ, Kendall CW, Marchie A, et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. Jenkins DJ, Jones PJ, Lamarche B, et al. Effect of a dietary portfolio of cholesterollowering foods given at 2 levels of intensity of dietary advice on serum lipids in hyperlipidemia: A randomized controlled trial. JAMA ;—9. Lovejoy JC, Most MM, Lefevre M, et al. Effect of diets enriched in almonds on insulin action and serum lipids in adults with normal glucose tolerance or type 2 diabetes. Jenkins DJ, Mirrahimi A, Srichaikul K, et al. Soy protein reduces serum cholesterol by both intrinsic and food displacement mechanisms. J Nutr ;s—11s. Tokede OA, Onabanjo TA, Yansane A, et al. Soya products and serum lipids: A meta-analysis of randomised controlled trials. Ras RT, Geleijnse JM, Trautwein EA. LDL-cholesterol-lowering effect of plant sterols and stanols across different dose ranges: Ameta-analysis of randomised controlled studies. Nordic Council. Nordic nutrition recommendations integrating nutrition and physical acitivity. Arhus, Denmark: Nordic Council of Ministers, Adamsson V, Reumark A, Fredriksson IB, et al. Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: A randomized controlled trial NORDIET. J Intern Med ;—9. Uusitupa M, Hermansen K, Savolainen MJ, et al. Effects of an isocaloric healthy Nordic diet on insulin sensitivity, lipid profile and inflammation markers in metabolic syndrome—arandomized study SYSDIET. J InternMed ;— Poulsen SK, Due A, Jordy AB, et al. Health effect of the NewNordic Diet in adults with increased waist circumference: A 6-mo randomized controlled trial. Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs lowfat diets onweight loss and cardiovascular risk factors: Ameta-analysis of randomized controlled trials. Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: One-year follow-up of a randomized trial. Shai I, Schwarzfuchs D, Henkin Y, et al. Weight Loss with a low-carbohydrate, Mediterranean, or low-fat diet. Dansinger ML, Gleason JA, Griffith JL, et al. Comparison of the Atkins, Ornish, WeightWatchers, and Zone diets for weight loss and heart disease risk reduction: A randomized trial. Sievenpiper JL, Kendall CW, Esfahani A, et al. Effect of non-oil-seed pulses on glycaemic control: A systematic reviewand meta-analysis of randomised controlled experimental trials in people with and without diabetes. Ha V, Sievenpiper JL, de Souza RJ, et al. Effect of dietary pulse intake on established therapeutic lipid targets for cardiovascular risk reduction: A systematic reviewandmeta-analysis of randomized controlled trials. CMAJ ;E— Jayalath VH, de Souza RJ, Sievenpiper JL, et al. Effect of dietary pulses on blood pressure: A systematic review and meta-analysis of controlled feeding trials. Am J Hypertens ;— Kim SJ, de Souza RJ, Choo VL, et al. Effects of dietary pulse consumption on body weight: A systematic review and meta-analysis of randomized controlled trials. Hosseinpour-Niazi S, Mirmiran P, Hedayati M, et al. Substitution of red meat with legumes in the therapeutic lifestyle change diet based on dietary advice improves cardiometabolic risk factors in overweight type 2 diabetes patients: A cross-over randomized clinical trial. Eur J Clin Nutr ;—7. Afshin A, Micha R, Khatibzadeh S, et al. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: A systematic review and meta-analysis. Health Canada. Ottawa: Health Products and Food Branch, Office of Nutrition and Promotion, Moazen S, Amani R, Homayouni Rad A, et al. Effects of freeze-dried strawberry supplementation on metabolic biomarkers of atherosclerosis in subjects with type 2 diabetes: A randomized double-blind controlled trial. Ann Nutr Metab ;— Hegde SV, Adhikari P, Nandini M, et al. Effect of daily supplementation of fruits on oxidative stress indices and glycaemic status in type 2 diabetes mellitus. Complement Ther Clin Pract ;— Imai S, Matsuda M, Hasegawa G, et al. Asia Pac J Clin Nutr ;—8. Shin JY, Kim JY, Kang HT, et al. Effect of fruits and vegetables on metabolic syndrome: A systematic reviewand meta-analysis of randomized controlled trials. Int J Food Sci Nutr ;— Petersen KS, Clifton PM, Blanch N, et al. Effect of improving dietary quality on carotid intima media thickness in subjects with type 1 and type 2 diabetes: A mo randomized controlled trial. Am J Clin Nutr ;—9. Viguiliouk E, Kendall CW, Blanco Mejia S, et al. Effect of tree nuts on glycemic control in diabetes: A systematic reviewand meta-analysis of randomized controlled dietary trials. Endocrinol Metab Clin North Am ;9:e Blanco Mejia S, Kendall CW, Viguiliouk E, et al. Effect of tree nuts onmetabolic syndrome criteria: A systematic reviewand meta-analysis of randomised controlled trials. BMJ Open ;4:e Sabate J, Oda K, Ros E. Nut consumption and blood lipid levels: A pooled analysis of 25 intervention trials. Flores-Mateo G, Rojas-Rueda D, Basora J, et al. Nut intake and adiposity:Metaanalysis of clinical trials. Whole grains—get the facts. Ottawa: Health Canada, Hollænder PL, Ross AB, Kristensen M. Whole-grain and blood lipid changes in apparently healthy adults: A systematic reviewand meta-analysis of randomized controlled studies. Bao L, Cai X, Xu M, et al. Effect of oat intake on glycaemic control and insulin sensitivity: A meta-analysis of randomised controlled trials. Chen M, Pan A, Malik VS, et al. Effects of dairy intake on body weight and fat: Ameta-analysis of randomized controlled trials. Benatar JR, Sidhu K, Stewart RA. Effects of high and lowfat dairy food on cardiometabolic risk factors: A meta-analysis of randomized studies. PLoS ONE ;8:e Maersk M, Belza A, Stødkilde-Jørgensen H, et al. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: A 6-mo randomized intervention study. Maki KC, Nieman KM, Schild AL, et al. Sugar-wweetened product consumption alters glucose homeostasis compared with dairy product consumption in men and women at risk of type 2 diabetes mellitus. Alexander DD, Bylsma LC, Vargas AJ, et al. Br J Nutr ; de Goede J, Soedamah-Muthu SS, Pan A, et al. Dairy consumption and risk of stroke: A systematic reviewand updated dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc ;5:pii: e Wolever TM, Hamad S, Chiasson JL, et al. Day-to-day consistency in amount and source of carbohydrate intake associated with improved blood glucose control in type 1 diabetes. J Am Coll Nutr ;—7. Clement S. Diabetes self-management education. Savoca MR, Miller CK, Ludwig DA. Food habits are related to glycemic control among people with type 2 diabetes mellitus. J AmDiet Assoc ;—6. Kalergis M, Schiffrin A, Gougeon R, et al. Impact of bedtime snack composition on prevention of nocturnal hypoglycemia in adults with type 1 diabetes undergoing intensive insulin management using lispro insulin before meals: A randomized, placebo-controlled, crossover trial. Arnold L, Mann JI, Ball MJ. Metabolic effects of alterations in meal frequency in type 2 diabetes. Leroux C, Brazeau AS, Gingras V, et al. Lifestyle and cardiometabolic risk in adults with type 1 diabetes: A review. Can J Diabetes ;—9. Delahanty LM, Nathan DM, Lachin JM, et al. Association of diet with glycated hemoglobin during intensive treatment of type 1 diabetes in the Diabetes Control and Complications Trial. Bell KJ, Smart CE, Steil GM, et al. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: Implications for intensive diabetes management in the continuous glucose monitoring era. Marran KJ, Davey B, Lang A, et al. Exponential increase in postprandial bloodglucose exposure with increasing carbohydrate loads using a linear carbohydrateto- insulin ratio. S Afr Med J ;—3. International Diabetes Federation, DAR International Alliance. Diabetes and Ramadan: Practical guidelines. Brussels: IDF IDF, Tunbridge FK, Home PD, MurphyM, et al. Does flexibility at mealtimes disturb blood glucose control on a multiple insulin injection regimen? Diabet Med ;—8. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: Dose adjustment for normal eating DAFNE randomised controlled trial. BMJ ; Scavone G, Manto A, Pitocco D, et al. Effect of carbohydrate counting andmedical nutritional therapy on glycaemic control in type 1 diabetic subjects: A pilot study. Diabet Med ;—9. Bergenstal RM, Johnson M, Powers MA, et al. Adjust to target in type 2 diabetes: Comparison of a simple algorithmwith carbohydrate counting for adjustment of mealtime insulin glulisine. Gillespie SJ, Kulkarni KD, Daly AE. Using carbohydrate counting in diabetes clinical practice. Kelley DE. Sugars and starch in the nutritional management of diabetes mellitus. Am J Clin Nutr ;s—64s. Rossi MC, Nicolucci A, Di Bartolo P, et al. Diabetes Interactive Diary: A new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: An open-label, international, multicenter, randomized study. Huckvale K, Adomaviciute S, Prieto JT, et al. Smartphone apps for calculating insulin dose: A systematic assessment. BMC Med ;13 1. List of permitted sweeteners list of permitted food additives. Gougeon R, Spidel M, Lee K, et al. Canadian Diabetes AssociationNationalNutrition Committee technical review: Nonnutritive intense sweeteners in diabetes management. Maki KC, Curry LL, Reeves MS, et al. Chronic consumption of rebaudioside A, a steviol glycoside, in men and women with type 2 diabetes mellitus. Food Chem Toxicol ;46 Suppl. Barriocanal LA, Palacios M, Benitez G, et al. Apparent lack of pharmacological effect of steviol glycosides used as sweeteners in humans. Apilot study of repeated exposures in some normotensive and hypotensive individuals and in Type 1 and Type 2 diabetics. Regul Toxicol Pharmacol ;— Azad NA,Mielniczuk L. A call for collaboration: Improving cardiogeriatric care. Can J Cardiol ;—4. Narain A, Kwok CS, Mamas MA. Soft drinks and sweetened beverages and the risk of cardiovascular disease and mortality: A systematic review and metaanalysis. Int J Clin Pract ;— Rogers PJ, Hogenkamp PS, de Graaf C, et al. Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int J Obes Lond ;— Wang YM, van Eys J. Nutritional significance of fructose and sugar alcohols. Annu Rev Nutr ;— Wolever TMS, Pickarz A, Hollands M, et al. Sugar alcohols and diabetes: A review. Heymsfield SB, van Mierlo CA, van der Knaap HC, et al. Weight management using a meal replacement strategy:Meta and pooling analysis from six studies. Li Z, Hong K, Saltsman P, et al. Long-term efficacy of soy-based meal replacements vs an individualized diet plan in obese type II DM patients: Relative effects on weight loss, metabolic parameters, and C-reactive protein. Cheskin LJ, Mitchell AM, Jhaveri AD, et al. Efficacy of meal replacements versus a standard food-based diet forweight loss in type 2 diabetes: A controlled clinical trial. Yip I, Go VL, DeShields S, et al. Liquid meal replacements and glycemic control in obese type 2 diabetes patients. Obes Res ;9 Suppl. McCargar LJ, Innis SM, Bowron E, et al. Effect of enteral nutritional products differing in carbohydrate and fat on indices of carbohydrate and lipid metabolism in patients with NIDDM. Mol Cell Biochem ;—9. Lansink M, van Laere KM, Vendrig L, et al. Lower postprandial glucose responses at baseline and after 4 weeks use of a diabetes-specific formula in diabetes type 2 patients. Diabetes Res Clin Pract ;—9. Stockwell T, Zhao J, Thomas G. Should alcohol policies aim to reduce total alcohol consumption? Newanalyses of Canadian drinking patterns. Addict Res Theory ;— Butt P, Beimess D, Stockwell T, et al. Alcohol and health in Canada: A summary of evidence and guidelines for low-risk drinking. Ottawa: Canadian Centre on Substance Abuse, Blomster JI, Zoungas S, Chalmers J, et al. The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes. Ahmed AT, Karter AJ,Warton EM, et al. The relationship between alcohol consumption and glycemic control among patients with diabetes: The Kaiser Permanente Northern California Diabetes Registry. J Gen Intern Med ;— Kerr D, Macdonald IA, Heller SR, et al. Alcohol causes hypoglycaemic unawareness in healthy volunteers and patients with type 1 insulin-dependent diabetes. Richardson T, Weiss M, Thomas P, et al. Day after the night before: Influence of evening alcohol on risk of hypoglycemia in patients with type 1 diabetes. Diabetes Care ;—2. Cheyne EH, Sherwin RS, Lunt MJ, et al. Influence of alcohol on cognitive performance during mild hypoglycaemia; implications for type 1 diabetes. Diabet Med ;—7. Pietraszek A, Gregersen S, Hermansen K. Alcohol and type 2 diabetes. A review. Gallagher A, Connolly V, Kelly WF. Alcohol consumption in patients with diabetes mellitus. Diabet Med ;—3. Carter S, Clifton PM, Keogh JB. The effects of intermittent compared to continuous energy restriction on glycaemic control in type 2 diabetes; a pragmatic pilot trial. Alabbood MH, Ho KW, Simons MR. The effect of Ramadan fasting on glycaemic control in insulin dependent diabetic patients: A literature review. Diabetes Metab Syndr ;—7. Chenhall C, Healthy Living Issue Group HLIG of the Pan-Canadian Public Health Network. Improving cooking and food preparation skills. A synthesis paper of the evidence to inform program and policy development. Ottawa: Canada Go, Desjardins E. Making something out of nothing: Food literacy among youth, young pregnant women and young parents who are at risk for poor health. Toronto: Public Health Ontario, Food skills: Definitions, influences and relationship with health. Cork, Ireland: SafeFood Food Safety Promotion Board , Slater J. Is cooking dead? The state of home economics food and nutrition education in a Canadian province. Int J Consum Stud ;— Nelson SA, Corbin MA, Nickols-Richardson SM. A call for culinary skills education in childhood obesity-prevention interventions: Current status and peer influences. J Acad Nutr Diet ;—6. Moubarac JC, Batal M, Martins AP, et al. Processed and ultra-processed food products: Consumption trends in Canada from to You should be taking your blood sugar at least two times per day to assess your control — a fasting blood sugar and a post prandial blood sugar. A fasting blood sugar is when you get a blood sugar reading when you first wake up, before you eat or drink anything. A post prandial blood sugar is when you get a blood sugar reading 2 hours after a meal. If you routinely get abnormally high numbers or abnormally low numbers, something is off and you need to reach out to your doctor immediately. Actively working with a Dietitian to monitor your diet, making adjustments as needed, and the ability to give you consistent feedback on your food choices and combinations is priceless when trying to achieve this goal. Also, working with your doctor so that they can monitor the decrease in medications, as well as approve adjustments in the amounts is also a crucial step in this process. Are you looking to achieve this goal? I hope you learned a thing or two on how to control your Diabetes by counting macros! If you need further support to reach your goals check out my Macros Nutrition Program. If you have any further questions feel free to comment below or email me at therealisticdietitian yahoo. More Macros Nutrition. hi i have active crohns ans was fasting all day so i could have somewhat of a life and eating at night. oh m diabetic now and also had my gall bladder removed. I can definitely help you to figure out a game plan in regards to what is going on with you. Your email address will not be published. Save my name, email, and website in this browser for the next time I comment. menu icon. search icon. Email Facebook Instagram LinkedIn Pinterest Twitter. Counting macros is often only seen as a solution for weight loss or an increase in muscle composition. While it absolutely can achieve those results, this approach can also be used to manage health complications and chronic disease. How to Select Carbohydrates for Meals and Snacks Are all carbohydrates created equal? The Power of Pairing Carbohydrates with a Fat and Protein Remember how I mentioned above that fiber slows down the release of sugar into the blood? |
| Food Order Has Significant Impact on Glucose and Insulin Levels | Newsroom | Weill Cornell Medicine | Kerr Bood, Macdonald IA, Heller Controll, et al. Fructose-containing sugars either in isocaloric substitution for starch or under ad libitum conditions Macronutrients and blood sugar control bliod demonstrated sufar adverse effect on lipoproteins LDL-C, TC, high-density lipoprotein cholesterol Mxcronutrientsbody weight or markers of glycemic control A1C, FBG or fasting blood insulin 71— User Tools Dropdown. Diabetes type 1 and 2 evidence-based nutrition practice guidelines for adults [article online], Sodium-glucose co-transporter-2 inhibitor use and dietary carbohydrate intake in Japanese individuals with type 2 diabetes: A randomized, open-label, 3-arm parallel comparative, exploratory study. Ottawa: Statistics Canada, Kulkarni K, Castle G, Gregory R, et al. |
| Understanding Carbs | We are much less concerned about proteins. Although they can be converted into blood sugar it happens when there is an overabundance of proteins and it does so in a slow and inefficient manner. When we digest carbohydrates, we brake them down to simple sugar molecules and absorb into the blood stream. As a result, our blood glucose levels goes up and insulin level goes up as well. Whether you eat a potato, a piece of bread or a cake, the result is the same — blood sugar rises rapidly and by a lot as these foods are predominantly carbs. When you eat high carbohydrate foods for breakfast, lunch and dinner and snack throughout the day you keep you glucose level and insulin level up. Here is a great database of foods and their carbohydrate content. Your cells, when exposed to high insulin level for a long time become less and less sensitive to it. Insulin resistance may result. Of concern for those following a low-CHO diet is the effectiveness of glucagon in the treatment of hypoglycemia. In a small study, people with type 1 diabetes treated with continuous subcutaneous insulin infusion CSII therapy following a low-CHO diet for 1 week had a blunted response to a glucagon bolus 40, The long-term sustainability and safety of these diets remains uncertain. The glycemic index GI provides an assessment of the quality of CHO-containing foods based on their ability to raise blood glucose BG To decrease the glycemic response to dietary intake, low-GI CHO foods are exchanged for high-GI CHO foods. Detailed lists can be found in the International Tables of Glycemic Index and Glycemic Load Values Systematic reviews and meta-analyses of randomized trials and large individual randomized trials of interventions replacing high-GI foods with low-GI foods have shown clinically significant improvements in glycemic control over 2 weeks to 6 months in people with type 1 or type 2 diabetes 44— This dietary strategy has also been shown to improve postprandial glycemia and reduce high-sensitivity C-reactive protein hsCRP over 1 year in people with type 2 diabetes 48 , reduce the number of hypoglycemic events over 24 to 52 weeks in adults and children with type 1 diabetes 47 and improve total cholesterol TC over 2 to 24 weeks in people with and without diabetes Irrespective of the comparator, recent systematic reviews and meta-analyses have confirmed the beneficial effect of low-GI diets on glycemic control and blood lipids in people with diabetes 49— Other lines of evidence extend these benefits. A systematic review and meta-analysis of prospective cohort studies inclusive of people with diabetes showed that high GI and high glycemic load GL diets are associated with increased incidence of cardiovascular disease CVD , when comparing the highest with the lowest exposures of GI and GL in women more than men over 6 to 25 years Dietary fibre includes the edible components of plant material that are resistant to digestion by human enzymes nonstarch polysaccharides and lignin, as well as associated substances. They include fibres from commonly consumed foods as well as accepted novel fibres that have been synthesized or derived from agricultural by-products Although these recommendations do not differentiate between insoluble and soluble fibres or viscous and nonviscous fibres within soluble fibre, the evidence supporting metabolic benefit is greatest for viscous soluble fibre from different plant sources e. beta-glucan from oats and barley, mucilage from psyllium, glucomannan from konjac mannan, pectin from dietary pulses, eggplant, okra and temperate climate fruits apples, citrus fruits, berries, etc. The addition of viscous soluble fibre has been shown to slow gastric emptying and delay the absorption of glucose in the small intestine, thereby improving postprandial glycemic control 54, Systematic reviews, meta-analyses of randomized controlled trials and individual randomized controlled trials have shown that different sources of viscous soluble fibre result in improvements in glycemic control assessed as A1C or fasting blood glucose FBG 56—58 and blood lipids 59— A lipid-lowering advantage is supported by Health Canada-approved cholesterol-lowering health claims for the viscous soluble fibres from oats, barley and psyllium 62— Despite contributing to stool bulking 65 , insoluble fibre has failed to show similar metabolic advantages in randomized controlled trials in people with diabetes 56,66, These differences between soluble and insoluble fibre are reflected in the EURODIAB prospective complications study, which demonstrated a protective association of soluble fibre that was stronger than that for insoluble fibre in relation to nonfatal CVD, cardiovascular CV mortality and all-cause mortality in people with type 1 diabetes However, this difference in the metabolic effects between soluble and insoluble fibre is not a consistent finding. A recent systematic review and meta-analysis of prospective cohort studies in people with and without diabetes did not show a difference in risk reduction between fibre types insoluble, soluble or fibre source cereal, fruit, vegetable Given this inconsistency, mixed sources of fibre may be the ideal strategy. Added sugars, especially from fructose-containing sugars high fructose corn syrup [HFCS], sucrose and fructose , have become a focus of intense public health concern. Fructose-containing sugars either in isocaloric substitution for starch or under ad libitum conditions have not demonstrated an adverse effect on lipoproteins LDL-C, TC, high-density lipoprotein cholesterol [HDL-C] , body weight or markers of glycemic control A1C, FBG or fasting blood insulin 71— Similar results have been seen for added fructose. Consumption of added fructose alone, in place of equal amounts of other sources of CHO mainly starch , does not have adverse effects on body weight 74,75 , BP 76 , fasting TG 77,78 , postprandial TG 79 , markers of fatty liver 80 or uric acid 75, In fact, it may even lower A1C 75,82,83 in most people with diabetes. Although HFCS has not been formally tested in controlled trials involving people with diabetes, there is no reason to expect that it would give different results than sucrose. Randomized controlled trials of head-to-head comparisons of HFCS vs. sucrose at doses from the 5th to 95th percentile of United States population intake have shown no differences between HFCS and sucrose over a wide range of cardiometabolic outcomes in participants with overweight or obesity without diabetes 84— Food sources of sugars may be a more important consideration than the type of sugar per se. A wide range of studies including people with and without diabetes have shown an adverse association of sugar-sweetened beverages SSBs with risk of hypertension and coronary heart disease when comparing the highest with the lowest levels of intake 88, This adverse relationship may be specific to SSBs as the same adverse relationship has not been shown for total sugars, sucrose, or fructose 90—97 , fructose-containing sugars from fruit 79,98 or food sources of added sugars, such as whole grains and dairy products yogurt 98— The DRIs do not specify an AI or RDA for total fat, monounsaturated fatty acids MUFA , saturated fatty acids SFA , or dietary cholesterol. The quality of fat type of fatty acids has been shown to be a more important consideration than the quantity of fat for CV risk reduction. Dietary strategies have tended to focus on the reduction of saturated fatty acids SFA and dietary cholesterol. These diets have shown improvements in lipids and other CV risk factors compared with higher SFA and cholesterol control diets More recent analyses have assessed the relation of different fatty acids with CV outcomes. A systematic review and meta-analysis of prospective cohort studies inclusive of people with diabetes showed that diets low in trans fatty acids TFA are associated with less coronary heart disease CHD Another systematic review and meta-analysis of randomized controlled clinical outcome trials involving people with and without diabetes showed that diets low in SFA decrease combined CV events Pooled analyses of prospective cohort studies and large individual cohort studies also suggest that replacement of saturated fatty acids with high quality sources of monounsaturated fatty acids MUFA from olive oil, canola oil, avocado, nuts and seeds, and high quality sources of carbohydrates from whole grains and low GI index carbohydrate foods is associated with decreased incidence of CHD , The food source of the saturated fatty acids being replaced, however, is another important consideration. Whereas adverse associations have been reliably established for meat as a food source of saturated fatty acids, the same has not been shown for some other food sources of saturated fatty acids e. such as dairy products and plant fats from palm and coconut A comprehensive review of long-chain omega-3 fatty acids LC-PUFAs eicosapentaenoic acid EPA and docosahexaenoic acid DHA from fish oils did not show an effect on glycemic control Large randomized clinical outcome trials of supplementation with omega-3 LC-PUFAs do not support their use in people with diabetes — The Outcome Reduction with Initial Glargine lntervention ORIGIN trial failed to show a CV or mortality benefit of supplementation with omega-3 LC-PUFA in 12, people with prediabetes or type 2 diabetes Subsequent systematic reviews and meta-analyses of randomized trials involving more than 75, participants with and without diabetes have failed to show a CV benefit of supplementation with long chain omega-3 PUFAs The Study of Cardiovascular Events in Diabetes ASCEND in 15, people with diabetes free of CV disease clinicaltrials. gov registration number NCT will provide more data on the outcomes of supplementation with omega-3 LC-PUFA in people with diabetes. Although supplementation with omega-3 LC-PUFA has not been shown to be beneficial, consumption of fish may be. The DRIs specify a recommended dietary allowance RDA for protein of 0. There is no evidence that the usual protein intake for most individuals 1 to 1. However, this intake in grams per kg per day should be maintained or increased with energy-reduced diets. Protein quality has been shown to be another important consideration. A systematic review and meta-analysis of randomized controlled trials showed that replacement of animal protein with sources of plant protein improved A1C, FPG and fasting insulin in people with type 1 and type 2 diabetes over a median follow up of 8 weeks People with diabetes who have CKD should target a level of intake that does not exceed the RDA of 0. When using a low-protein diet, harm due to malnutrition should not be ignored Both the quantity and quality high biological value of protein intake must be optimized to meet requirements for essential amino acids, necessitating adequate clinical and laboratory monitoring of nutritional status in the individual with diabetes and CKD. Greater incorporation of plant sources of protein may also require closer monitoring of potassium as CKD progresses. The ideal macronutrient distribution for the management of diabetes can be individualized. Based on evidence for chronic disease prevention and adequacy of essential nutrients, the DRIs recommend acceptable macronutrient distribution ranges AMDRs for macronutrients as a percentage of total energy. There may be a benefit of substituting fat as MUFA for carbohydrate Similarly, the replacement of refined high-GI CHO with MUFA The effect of the replacement of fat with CHO depends on the quality of the CHO and the fat. Whereas the replacement of fat with refined high-GI CHO results in worsening of metabolic parameters in people with type 2 diabetes , the replacement of saturated fatty acids with low-GI CHO or whole grain sources is associated with decreased incident CHD in people with and without diabetes , When protein is used to replace CHO, as in a high-protein diet, benefit has only been demonstrated when high-GI CHO are replaced. These differences were seen despite similar weight loss with normal renal function being maintained Rather, it was adherence to any 1 diet and the degree of energy restriction, not the variation in diet macronutrient composition, that was associated with the long-term improvement in glycemic control and cardiometabolic risk factors Adjustments in medication type and dosage may be required when embarking on a different macronutrient distribution or energy reduction to avoid hypoglycemia. Intensive lifestyle intervention ILI programs in diabetes usually consist of behavioural interventions combining dietary modification and increased physical activity. An interprofessional team, including registered dietitians, nurses and kinesiologists, usually leads the ILl programs, with the intensity of follow up varying from weekly to every 3 months with gradually decreasing contact as programs progress. Large, randomized clinical trials have shown benefit of ILl programs using different lifestyle approaches in diabetes. Twenty-year follow up of the China Da Qing Diabetes Prevention Outcome Study showed that 6 years of an ILl program targeting an increase in vegetable intake, decrease in alcohol and simple sugar intake, weight loss through energy restriction in participants with overweight or obesity, and an increase in leisure time physical activity e. However, it should be noted that analysis after 8 years showed that initial weight loss was attributable to reduction in both fat and lean mass, whereas weight regain was attributable only to fat mass, with continued decline in lean mass Improvements in glycemic control and CV risk factors BP, TG and HDL-C were greatest at 1 year and diminished over time with the most sustainable reductions being in A1C, fitness and systolic BP In , the Look AHEAD trial was stopped early as it was determined that 11 years of an ILl did not decrease the occurrence of CV events compared to the control group and further intervention was unlikely to change this result. It was noted, however, that both groups had a lower number of CV events compared to previous studies of people with diabetes. Other studies of ILI have shown similar results , Although the available trials suggest an overall short-term benefit of different ILl programs in people with diabetes, the feasibility of implementing an ILl program will depend on the availability of resources and access to an interprofessional team. Effects attenuate within 8 years and do not appear to provide lasting CV protection. A variety of dietary patterns have been studied for people with prediabetes and diabetes. An individual's values, preferences and treatment goals will influence the decision to use these dietary patterns. A Mediterranean diet primarily refers to a plant-based diet first described in the s General features include high consumption of fruits, vegetables, legumes, nuts, seeds, cereals and whole grains; moderate-to-high consumption of olive oil as the principal source of fat ; low-to-moderate consumption of dairy products, fish and poultry; low consumption of red meat; and low-to-moderate consumption of wine, mainly during meals , Systematic reviews and meta-analyses of randomized controlled feeding trials have shown that a Mediterranean-style dietary pattern improves glycemic control 50, , and improves systolic BP, TC, HDL-C, TC:HDL-C ratio and TG in type 2 diabetes , A low-CHO Mediterranean-style diet reduced A1C, delayed the need for antihyperglycemic drug therapy and increased rates of diabetes remission compared with a low-fat diet in overweight individuals with newly diagnosed type 2 diabetes at 8 years Compared with a diet based on the American Diabetes Association recommendations, both traditional and low-CHO Mediterranean-style diets were shown to decrease A1C and TG, whereas only the low-CHO Mediterranean-style diet improved LDL-C and HDL-C at 1 year in persons with overweight and type 2 diabetes Both the extra-virgin olive oil and mixed nuts arms of the PREDIMED trial also reduced risk of incident retinopathy. No effect on nephropathy was detected Vegetarian dietary patterns include lacto-ovovegetarian, lactovegetarian, ovovegetarian and vegan dietary patterns. A low-fat, ad libitum vegan diet has been shown to be just as beneficial as conventional American Diabetes Association dietary guidelines in promoting weight loss and improving fasting BG and lipids over 74 weeks in adults with type 2 diabetes and, when taking medication changes into account, the vegan diet improved glycemia and plasma lipids more than the conventional diet On both diets, weekly or biweekly nutrition and cooking instruction was provided by a dietitian or cooking instructor Similarly, a calorie-restricted vegetarian diet was shown to improve BMI and LDL-C more than a conventional diet in people with type 2 diabetes Subsequent systematic reviews and meta-analyses of the available randomized controlled trials have shown that vegetarian and vegan dietary patterns resulted in clinically meaningful improvements in A1C and FBG in people with type 1 and type 2 diabetes over 4 to 74 weeks , , as well as body weight and blood lipids in people with and without diabetes over 3 to 74 weeks. A systematic review and meta-analysis of prospective cohort and cross-sectional observational studies showed a protective association between vegetarian dietary patterns and incident fatal and nonfatal CHD Dietary approaches to reducing BP have focused on sodium reduction and the Dietary Approaches to Stop Hypertension DASH dietary pattern. The DASH dietary pattern does not target sodium reduction but rather emphasizes vegetables, fruits and low-fat dairy products, and includes whole grains, poultry, fish and nuts. It contains smaller amounts of red and processed meat, sweets, sugar-containing beverages, total and saturated fat, and cholesterol, and larger amounts of potassium, calcium, magnesium, dietary fibre and protein than typical Western diets , The DASH dietary pattern has been shown to lower systolic and diastolic BP compared with a typical American diet matched for sodium intake in people with and without hypertension, inclusive of people with well-controlled diabetes , In addition to BP-lowering benefit, a systematic review and meta-analysis of randomized controlled trials showed that a DASH dietary pattern lowered lipids, including LDL-C in people with and without hypertension, some of whom had metabolic syndrome or diabetes A systematic review and meta-analysis of prospective cohort studies that included people with diabetes showed that adherence to a DASH dietary pattern was associated with a reduction in incident CVD These small effects combine to provide a meaningful overall reduction in LDL-C lowering. Although the Portfolio dietary pattern has not been formally tested in people with diabetes, each component has been shown individually to lower LDL-C in systematic reviews and meta-analyses of randomized controlled trials inclusive of people with diabetes 57,59—61,— The results of the Combined Portfolio Diet and Exercise Study PortfolioEx trial , a 3-year multicentre randomized controlled trial of the effect of the Portfolio Diet plus exercise on atherosclerosis, assessed by magnetic resonance imaging MRI in high CV risk people ClinicalTrials. gov Identifier, NCT , will provide important new data in people with diabetes, as approximately one-half of the participants will have type 2 diabetes. The Nordic Diet was developed as a Nordic translation of the Mediterranean, Portfolio, DASH and NCEP dietary patterns, using foods typically consumed as part of a traditional Nordic diet in the context of Nordic Nutrition Recommendations The Nordic Diet has not been studied in people with diabetes; however, 3 high-quality randomized controlled trials have studied the effect of a Nordic Diet on glycemic control and other relevant cardiometabolic outcomes in people with central obesity or metabolic syndrome. These have shown improvements in body weight, insulin resistance, and lipids, including the therapeutically relevant LDL-C and non-HDL-C — Numerous popular weight-loss diets providing a range of macronutrient profiles are available to people with diabetes. Furthermore, the Mediterranean-style diet had a more favourable effect on FPG at 2 years in the subgroup of participants with type 2 diabetes Dietary pulses, the dried seeds of nonoil seed legumes, include beans, peas, chickpeas, and lentils. This taxonomy does not include the oil-seed legumes soy, peanuts or fresh legumes peas, beans. A systematic review and meta-analysis of prospective cohort studies, inclusive of people with diabetes, showed that the intake of 4 weekly g servings of legumes is associated with decreased incident total CHD Eating Well with Canada's Food Guide recommends up to 7 to 10 servings of fruit and vegetables per day Individual randomized controlled trials have shown that supplementation with fresh or freeze dried fruits improves A1C over 6 to 8 weeks in individuals with type 2 diabetes , A novel and simple technique of encouraging intake of vegetables first and other CHOs last at each meal was successful in achieving better glycemic control A1C than an exchange-based meal plan after 24 months of follow up in people with type 2 diabetes A systematic review and meta-analysis of randomized controlled trials also showed that fruit and vegetables provided as either foods or supplements improved diastolic BP over 6 weeks to 6 months in individuals with the metabolic syndrome, some of whom had prediabetes In people with type 1 and type 2 diabetes, an intervention to increase the intake of fruit, vegetables and dairy that only succeeded in increasing the intake of fruits and vegetables, led to a similar improvement in diastolic blood pressure and to a clinically meaningful regression in carotid intima medial thickness over 1 year Although there is a need to understand better the advantages of different fruit and vegetables in people with diabetes, higher intake of total fruit and vegetables remains an important part of all healthy dietary patterns. Nuts include both peanuts a legume and tree nuts, such as almonds, walnuts, pistachios, pecans, Brazil nuts, cashews, hazelnuts, macadamia nuts and pine nuts. An individual patient-level meta-analysis of 25 nut intervention trials of the effect of nuts on lipid outcomes in people with normolipidemia or hypercholesterolemia including 1 trial in people with type 2 diabetes also showed a dose-dependent reduction in blood lipids, including the established therapeutic target LDL-C A systematic review and meta-analysis of prospective cohort studies in people with and without diabetes also showed that the intake of 4 weekly Despite concerns that the high energy density of nuts may contribute to weight gain, systematic reviews of randomized controlled trials have failed to show an adverse effect of nuts on body weight and measures of adiposity when nuts are consumed as part of balanced, healthy dietary patterns , Health Canada defines whole grains as those that contain all 3 parts of the grain kernel bran, endosperm, germ in the same relative proportions as they exist in the intact kernel. Health Canada recommends that at least half of all daily grain servings are consumed from whole grains Sources of whole grains include both the cereal grains e. wheat, rice, oats, barley, corn, wild rice, and rye and pseudocereal grains e. quinoa, amaranth and buckwheat but not oil seeds e. soy, flax, sesame seeds, poppy seeds. Systematic reviews and meta-analyses of randomized controlled trials have shown that whole grain interventions, specifically with whole grain sources containing the viscous soluble fibre beta-glucan, such as oats and barley, improve lipids, including TG and LDL-C, in people with and without diabetes over 2 to 16 weeks of follow up Whole grains have also been shown to improve glycemic control. Whole grains from barley have shown improvements in fasting glucose in people with and without diabetes 57 and whole grains from oats have shown improvements in A1C and FPG in the subgroup with type 2 diabetes In contrast, these advantages have not been seen for whole grain sources from whole wheat or wheat bran in people with type 2 diabetes 56,66, Systematic reviews and meta-analyses of prospective cohort studies have shown a protective association of total whole grains where wheat is the dominant source and total cereal fibre as a proxy of whole grains with incident CHD in people with and without diabetes 69, Although higher intake of all whole grains remains advisable especially from oats and barley , more research is needed to understand the role of different sources of whole grains in people with diabetes. Dairy products broadly include low- and full-fat milk, cheese, yogurt, other fermented products and ice cream. Evidence for the benefit of specific dairy products as singular interventions in the management of diabetes is inconclusive. Systematic reviews and meta-analyses of randomized controlled trials of the effect of diets rich in either low- or full-fat dairy products have not shown any clear advantages for body weight, body fat, waist circumference, FPG or BP across individuals with different metabolic phenotypes otherwise healthy, with overweight or obesity, or metabolic syndrome , The comparator, however, may be an important consideration. Individual randomized controlled trials, which have assessed the effect of dairy products in isocaloric substitution with SSBs and foods, have shown advantages for visceral adipose tissue, systolic blood pressure and triglycerides in individuals with overweight or obesity over 6 months and markers of insulin resistance in people with prediabetes over 6 weeks Other evidence from observational studies is suggestive of a weight loss and CV benefit. Large pooled analyses of the Harvard cohorts have shown that higher intakes of yogurt are associated with decreased body weight over 12 to 20 years of follow up in people with and without diabetes Systematic reviews and meta-analyses of prospective cohort studies inclusive of people with diabetes have also shown a protective association of cheese with incident CHD; low-fat dairy products with incident CHD; and total, low-fat, and full-fat dairy products, and total milk with incident stroke over 5 to 26 years of follow up , For persons on insulin, consistency in CHO intake and spacing and regularity in meal consumption may help control BG levels — Inclusion of snacks as part of a person's meal plan should be individualized based on meal spacing, metabolic control, treatment regimen and risk of hypoglycemia, and should be balanced against the potential risk of weight gain , The nutritional recommendations that reduce CV risk apply to both type 1 and type 2 diabetes. Studies have shown that people with type 1 diabetes tend to consume diets that are low in fibre, and high in protein and saturated fat In addition, it was shown in the Diabetes Control and Complications Trial DCCT , intensively treated individuals with type 1 diabetes showed worse diabetes control with diets high in total and saturated fat and low in CHO Meals high in fat and protein may require additional insulin and, for those using CSII, the delivery of insulin may be best given over several hours Algorithms for improved bolusing are under investigation. Heavy CHO loads greater than 60 g have been shown to result in greater glucose area under the curve and some risk of late postprandial hypoglycemia People with type 1 diabetes or type 2 diabetes requiring insulin, using a basal-bolus regimen, should adjust their insulin based on the CHO content of their meals, and inject their insulin within 15 minutes of eating with rapid-acting insulin analogues and just prior to and if required up to 20 minutes after eating with faster-acting insulin aspart for optimal match between rapid insulin and glycemic meal rise see Glycemic Management of Type 1 Diabetes in Adults chapter, p. Intensive insulin therapy regimens that include multiple injections of rapid-acting insulin matched to CHO allow for flexibility in meal size and frequency , Improvements in A1C, BG and quality of life, as well as less requirement for insulin, can be achieved when individuals with type 1 diabetes or type 2 diabetes receive education on matching insulin to CHO content e. CHO counting , In doing so, dietary fibre and sugar alcohol should be subtracted from total CHO. They also improved individual quality of life and treatment satisfaction Sugar substitutes, which include high-intensity sweeteners and sugar alcohols, are regulated as food additives in Canada. Health Canada has set acceptable daily intake ADI values, which are expressed on a body weight basis and are considered safe daily intake levels over a lifetime Table 2. These levels are considered high and are rarely achieved. Most have been shown to be safe when used by people with diabetes — ; however, there are limited data on the newer sweeteners, such as neotame and thaumatin in people with diabetes. Although systematic reviews and meta-analyses of prospective cohort studies inclusive of people with diabetes have shown an adverse association of non-nutritive sweetened beverages with weight gain, CVD and stroke, it is well recognized that these data are at high risk of reverse causality , The evidence from systematic reviews and meta-analyses of randomized controlled trials, which give a better protection against bias, have shown a weight loss benefit when non-nutritive sweeteners are used to displace excess calories from added sugars especially from SSBs in overweight children and adults without diabetes , a benefit that has been shown to be similar to that seen with other interventions intended to displace excess calories from added sugars, such as water Sugar alcohols approved for use in Canada include: erythritol, isomalt, lactitol, maltitol, mannitol, sorbitol, xylitol. There is no ADI for sugar alcohols except for erythritol as their use is considered self-limiting due to the potential for adverse gastrointestinal symptoms. They vary in the degree to which they are absorbed, and their conversion rate to glucose is slow, variable and usually minimal, and may have no significant effect on BG. Thus, matching rapid-acting insulin to the intake of sugar alcohols is not recommended Weight loss programs for people with diabetes may use partial meal replacement plans. Commercially available, portion-controlled, vitamin- and mineral-fortified meal replacement products usually replace 1 or 2 meals per day in these plans. Randomized controlled feeding trials have shown partial meal replacement plans result in comparable or increased , weight loss compared with conventional reduced-calorie diets for up to 1 year with maintenance up to 86 weeks in people with type 2 diabetes and overweight. This weight loss results in greater improvements in glycemic control over 3 months to 34 weeks , and reductions in the need for antihyperglycemic medications up to 1 year without an increase in hypoglycemic or other adverse events — Meal replacements with differing macronutrient compositions designed for people with diabetes have shown no clear advantage, although studies are lacking , The same precautions regarding alcohol consumption in the general population apply to people with diabetes For people with type 1 diabetes, moderate consumption of alcohol with, or 2 or 3 hours after, an evening meal may result in delayed hypoglycemia the next morning after breakfast or as late as 24 hours after alcohol consumption , and may impede cognitive performance during mild hypoglycemia The same concern may apply to sulphonylurea- and insulin-treated individuals with type 2 diabetes Health-care professionals should discuss alcohol use with people with diabetes to inform them of the potential weight gain and risks of hypoglycemia People with diabetes should be encouraged to meet their nutritional needs by consuming a well-balanced diet by following Eating Well with Canada's Food Guide Routine vitamin and mineral supplementation is generally not recommended. Supplementation with folic acid 0. The need for further vitamin and mineral supplements should be assessed on an individual basis. As vitamin and mineral supplements are regulated as natural health products NHP in Canada, the evidence for their therapeutic role in diabetes has been reviewed in the Complementary and Alternative Medicine for Diabetes chapter, p. Within the lay literature, intermittent energy restriction strategies for weight loss have become more prevalent. To date, there is limited evidence for these approaches with people with type 2 diabetes. Traditionally, Muslims with type 1 and insulin-requiring type 2 diabetes have been exempted from participation in Ramadan fasting, due to concerns of hypo- and hyperglycemia. Similarly, people on non-insulin antihyperglycemic agents associated with hypoglycemia are also considered high risk for fasting. People with diabetes who wish to participate in Ramadan fasting are encouraged to consult with their diabetes health-care team 1 to 2 months prior to the start of Ramadan. While evidence for the impact of Ramadan fasting in individuals with type 1 diabetes is limited, the literature suggests that in people with well-controlled type 1 diabetes, complications from fasting are rare. A reduction in the total daily dose of insulin can reduce the incidence of hypoglycemia. CSII therapy or the use of multiple daily injections with rapid-acting insulin taken with meals and basal insulin, combined with frequent self-monitoring of blood glucose SMBG can help reduce the risk of hypo- and hyperglycemia. Individuals with a history of severe hypoglycemia or hypoglycemia unawareness should be discouraged from participating in Ramadan fasting , pdf While there is no universally agreed upon definition of food skills, it is generally thought that they are interdependent technical, mechanical, conceptual and perceptual skills that are necessary to safely select and plan, prepare, and store nutritious and culturally-acceptable meals and snacks — Several studies suggest that food preparation and cooking skills are declining globally ,, Over the past several decades, in Canada, there has been an increase in processed, pre-prepared and convenience foods being purchased and assembled rather than meals being prepared using whole, basic ingredients To our knowledge, there are no studies that have investigated food skills in people with diabetes. Nevertheless, targeted interventions to improve the food skills of people living with diabetes are prudent given that food is central to managing glycemic control. People with type 1 diabetes may be taught how to match insulin to carbohydrate quantity and quality [Grade C, Level 2 ] or they may maintain consistency in carbohydrate quantity and quality [Grade D, Consensus]. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Chan reports grants from Danone Institute, Canadian Foundation for Dietetic Research, Alberta Livestock and Meat Agency, Dairy Farmers of Canada, Alberta Pulse Growers, and Western Canada Grain Growers, outside the submitted work; in addition, Dr. Chan has a patent No. Catherine Freeze reports personal fees from Dietitians of Canada and Government of Prince Edward Island, outside the submitted work. No other authors have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Ethnocultural Diversity Approach to Nutrition Therapy Energy Macronutrients Intensive Lifestyle Intervention Dietary Patterns Diets Emphasizing Specific Foods Special Considerations for People with Type 1 Diabetes and Type 2 Diabetes on Insulin Other Considerations Other Relevant Guidelines Author Disclosures. Key Messages People with diabetes should receive nutrition counselling by a registered dietitian. Nutrition therapy can reduce glycated hemoglobin A1C by 1. Reduced caloric intake to achieve and maintain a healthier body weight should be a treatment goal for people with diabetes with overweight or obesity. The macronutrient distribution is flexible within recommended ranges and will depend on individual treatment goals and preferences. Replacing high-glycemic-index carbohydrates with low-glycemic-index carbohydrates in mixed meals has a clinically significant benefit for glycemic control in people with type 1 and type 2 diabetes. Consistency in spacing and intake of carbohydrate intake and in spacing and regularity in meal consumption may help control blood glucose and weight. Intensive healthy behaviour interventions in people with type 2 diabetes can produce improvements in weight management, fitness, glycemic control and cardiovascular risk factors. A variety of dietary patterns and specific foods have been shown to be of benefit in people with type 1 and type 2 diabetes. People with diabetes should be encouraged to choose the dietary pattern that best aligns with their values, preferences and treatment goals, allowing them to achieve the greatest adherence over the long term. Key Messages for People with Diabetes It is natural to have questions about what food to eat. A registered dietitian can help you develop a personalized meal plan that considers your culture and nutritional preferences to help you achieve your blood glucose and weight management goals. Food is key in the management of diabetes and reducing the risk of heart attack and stroke. Try to prepare more of your meals at home and use fresh unprocessed ingredients. Try to prepare meals and eat together as a family. This is a good way to model healthy food behaviours to children and teenagers, which could help reduce their risk of becoming overweight or developing diabetes. With prediabetes and recently diagnosed type 2 diabetes, weight loss is the most important and effective dietary strategy if you have overweight or obesity. There are many strategies that can help with weight loss. The best strategy is one that you are able to maintain long term. Adoption of diabetes-friendly eating habits can help manage your blood glucose levels as well as reduce your risk for developing heart and blood vessel disease for those with either type 1 or type 2 diabetes. Select whole and less refined foods instead of processed foods, such as sugar-sweetened beverages, fast foods and refined grain products. Pay attention to both carbohydrate quality and quantity. Include low-glycemic-index foods, such as legumes, whole grains, and fruit and vegetables. These foods can help control blood glucose and cholesterol levels. Consider learning how to count carbohydrates as the quantity of carbohydrate eaten at one time is usually important in managing diabetes. Select unsaturated oils and nuts as the preferred dietary fats. Choose lean animal proteins. Select more vegetable protein. The style of eating that works well for diabetes may be described as a Mediterranean style diet, Nordic style diet, DASH diet or vegetarian style diet. All of these diets are rich in protective foods and have been shown to help manage diabetes and cardiovascular disease. They all contain the key elements of a diabetes-friendly diet. Introduction Nutrition therapy and counselling are an integral part of the treatment and self-management of diabetes. Ethnocultural Diversity Canada is a country rich in ethnocultural diversity. Approach to Nutrition Therapy Nutrition therapy should be individualized, regularly evaluated, reinforced in an intensive manner 11,12 , and should incorporate self-management education Figure 1 Nutritional management of hyperglycemia in type 2 diabetes. A1C , glycated hemoglobin. Macronutrients The ideal macronutrient distribution for the management of diabetes may vary, depending on the quality of the various macronutrients, the goals of the dietary treatment regimen and the individual's values and preferences. Carbohydrate CHO broadly include available CHO from starches and sugars and unavailable CHO from fibre. Glycemic Index The glycemic index GI provides an assessment of the quality of CHO-containing foods based on their ability to raise blood glucose BG Dietary fibre Dietary fibre includes the edible components of plant material that are resistant to digestion by human enzymes nonstarch polysaccharides and lignin, as well as associated substances. Sugars Added sugars, especially from fructose-containing sugars high fructose corn syrup [HFCS], sucrose and fructose , have become a focus of intense public health concern. Fat The DRIs do not specify an AI or RDA for total fat, monounsaturated fatty acids MUFA , saturated fatty acids SFA , or dietary cholesterol. Protein The DRIs specify a recommended dietary allowance RDA for protein of 0. Macronutrient substitutions The ideal macronutrient distribution for the management of diabetes can be individualized. Intensive Lifestyle Intervention Intensive lifestyle intervention ILI programs in diabetes usually consist of behavioural interventions combining dietary modification and increased physical activity. Dietary Patterns A variety of dietary patterns have been studied for people with prediabetes and diabetes. Mediterranean dietary patterns A Mediterranean diet primarily refers to a plant-based diet first described in the s Vegetarian dietary patterns Vegetarian dietary patterns include lacto-ovovegetarian, lactovegetarian, ovovegetarian and vegan dietary patterns. DASH and low-sodium dietary patterns Dietary approaches to reducing BP have focused on sodium reduction and the Dietary Approaches to Stop Hypertension DASH dietary pattern. Nordic dietary patterns The Nordic Diet was developed as a Nordic translation of the Mediterranean, Portfolio, DASH and NCEP dietary patterns, using foods typically consumed as part of a traditional Nordic diet in the context of Nordic Nutrition Recommendations Popular weight-loss diets Numerous popular weight-loss diets providing a range of macronutrient profiles are available to people with diabetes. Diets Emphasizing Specific Foods Dietary pulses and legumes Dietary pulses, the dried seeds of nonoil seed legumes, include beans, peas, chickpeas, and lentils. Fruit and vegetables Eating Well with Canada's Food Guide recommends up to 7 to 10 servings of fruit and vegetables per day Nuts Nuts include both peanuts a legume and tree nuts, such as almonds, walnuts, pistachios, pecans, Brazil nuts, cashews, hazelnuts, macadamia nuts and pine nuts. Whole grains Health Canada defines whole grains as those that contain all 3 parts of the grain kernel bran, endosperm, germ in the same relative proportions as they exist in the intact kernel. Dairy products Dairy products broadly include low- and full-fat milk, cheese, yogurt, other fermented products and ice cream. Special Considerations for People with Type 1 Diabetes and Type 2 Diabetes on Insulin For persons on insulin, consistency in CHO intake and spacing and regularity in meal consumption may help control BG levels — Other Considerations Non-nutritive sweeteners Sugar substitutes, which include high-intensity sweeteners and sugar alcohols, are regulated as food additives in Canada. Meal replacements Weight loss programs for people with diabetes may use partial meal replacement plans. Alcohol The same precautions regarding alcohol consumption in the general population apply to people with diabetes Vitamin and mineral supplements People with diabetes should be encouraged to meet their nutritional needs by consuming a well-balanced diet by following Eating Well with Canada's Food Guide Fasting and diabetes Within the lay literature, intermittent energy restriction strategies for weight loss have become more prevalent. Ramadan Traditionally, Muslims with type 1 and insulin-requiring type 2 diabetes have been exempted from participation in Ramadan fasting, due to concerns of hypo- and hyperglycemia. Food skills While there is no universally agreed upon definition of food skills, it is generally thought that they are interdependent technical, mechanical, conceptual and perceptual skills that are necessary to safely select and plan, prepare, and store nutritious and culturally-acceptable meals and snacks — Recommendations People with diabetes should receive nutrition counselling by a registered dietitian to lower A1C levels [Grade B, Level 2 3 , for those with type 2 diabetes; Grade D, Consensus, for type 1 diabetes] and to reduce hospitalization rates [Grade C, Level 3 8 ]. Nutrition education may be delivered in either a small group or one-on-one setting [Grade B, Level 2 18 ]. Group education should incorporate adult education principles, such as hands-on activities, problem solving, role playing and group discussions [Grade B, Level 2 19 ]. Individuals with diabetes should be encouraged to follow Eating Well with Canada's Food Guide in order to meet their nutritional needs [Grade D, Consensus]. In people with overweight or obesity with diabetes, a nutritionally balanced, calorie-reduced diet should be followed to achieve and maintain a lower, healthier body weight [Grade A, Level 1A 29,30 ]. An intensive healthy behaviour intervention program, combining dietary modification and increased physical activity, may be used to achieve weight loss, improve glycemic control and reduce CV risk [Grade A, Level 1A 30 ]. People with type 2 diabetes should maintain regularity in timing and spacing of meals to optimize glycemic control [Grade D, Level 4 ]. Adults with diabetes should select carbohydrate food sources with a low-GI to help optimize glycemic control [Grade B, Level 2 46,47 for type 1 diabetes; Grade B, Level 2 32,44 for type 2 diabetes], to improve LDL-C [Grade C, Level 3 49 ] and to decrease CV risk [Grade D, Level 4 52 ]. The following dietary patterns may be considered in people with type 2 diabetes, incorporating patient preferences, including: Mediterranean-style dietary pattern to reduce major CV events [Grade A, Level 1A ] and improve glycemic control [Grade B, Level 2 50, ]. Vegan or vegetarian dietary pattern to improve glycemic control [Grade B, Level 2 , ], body weight [Grade C, Level 3 ], and blood lipids, including LDL-C [Grade B, Level 2 ] and reduce myocardial infarction risk [Grade B, Level 2 ]. DASH dietary pattern to improve glycemic control [Grade C, Level 2 ], BP [Grade D, Level 4 — ], and LDL-C [Grade B, Level 2 , ] and reduce major CV events [Grade B, Level 3 ]. Dietary patterns emphasizing dietary pulses e. beans, peas, chickpeas, lentils to improve glycemic control [Grade B, Level 2 ], systolic BP [Grade C, Level 2 ] and body weight [Grade B, Level 2 ]. Dietary patterns emphasizing fruit and vegetables to improve glycemic control [Grade B, Level 2 , ] and reduce CV mortality [Grade C, Level 3 79 ]. Dietary patterns emphasizing nuts to improve glycemic control [Grade B, Level 2 ], and LDL-C [Grade B, Level 2 ]. Other Relevant Guidelines Chapter 7. Self-Management Education and Support Chapter Physical Activity and Diabetes Chapter Weight Management in Diabetes Chapter Complementary and Alternative Medicine for Diabetes Chapter Dyslipidemia Chapter Treatment of Hypertension Chapter Type 1 Diabetes in Children and Adolescents Chapter Type 2 Diabetes in Children and Adolescents Chapter Diabetes and Pregnancy Chapter Diabetes in Older People Chapter Type 2 Diabetes and Indigenous Peoples. Author Disclosures Dr. References Pastors JG,WarshawH, Daly A, et al. The evidence for the effectiveness of medical nutrition therapy in diabetes management. Diabetes Care ;— Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care ;—7. Franz MJ, Monk A, Barry B, et al. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: A randomized, controlled clinical trial. J Am Diet Assoc ;— Kulkarni K, Castle G, Gregory R, et al. Nutrition practice guidelines for type 1 diabetes mellitus positively affect dietitian practices and patient outcomes. The Diabetes Care and Education Dietetic Practice Group. J Am Diet Assoc ;—70, quiz Gaetke LM, Stuart MA, Truszczynska H. A single nutrition counseling session with a registered dietitian improves short-term clinical outcomes for rural Kentucky patients with chronic diseases. Imai S, Kozai H, Matsuda M, et al. Intervention with delivery of diabetic meals improves glycemic control in patients with type 2 diabetes mellitus. J Clin Biochem Nutr ;— Huang MC, Hsu CC, Wang HS, et al. Prospective randomized controlled trial to evaluate effectiveness of registered dietitian-led diabetes management on glycemic and diet control in a primary care setting in Taiwan. Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. A prospective study of dietary carbohydrate quantity and quality in relation to risk of ovulatory infertility. Eur J Clin Nutr. Higginbotham S, Zhang ZF, Lee IM, et al. J Natl Cancer Inst. Liu S, Willett WC. Dietary glycemic load and atherothrombotic risk. Curr Atheroscler Rep. Willett W, Manson J, Liu S. Glycemic index, glycemic load, and risk of type 2 diabetes. Livesey G, Taylor R, Livesey H, Liu S. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Mirrahimi A, de Souza RJ, Chiavaroli L, et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts. J Am Heart Assoc. Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: Buyken, AE, Goletzke, J, Joslowski, G, Felbick, A, Cheng, G, Herder, C, Brand-Miller, JC. Association between carbohydrate quality and inflammatory markers: systematic review of observational and interventional studies. The American Journal of Clinical Nutrition Am J Clin Nutr. AlEssa H, Bupathiraju S, Malik V, Wedick N, Campos H, Rosner B, Willett W, Hu FB. Carbohydrate quality measured using multiple quality metrics is negatively associated with type 2 diabetes. The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products. Skip to content The Nutrition Source. |
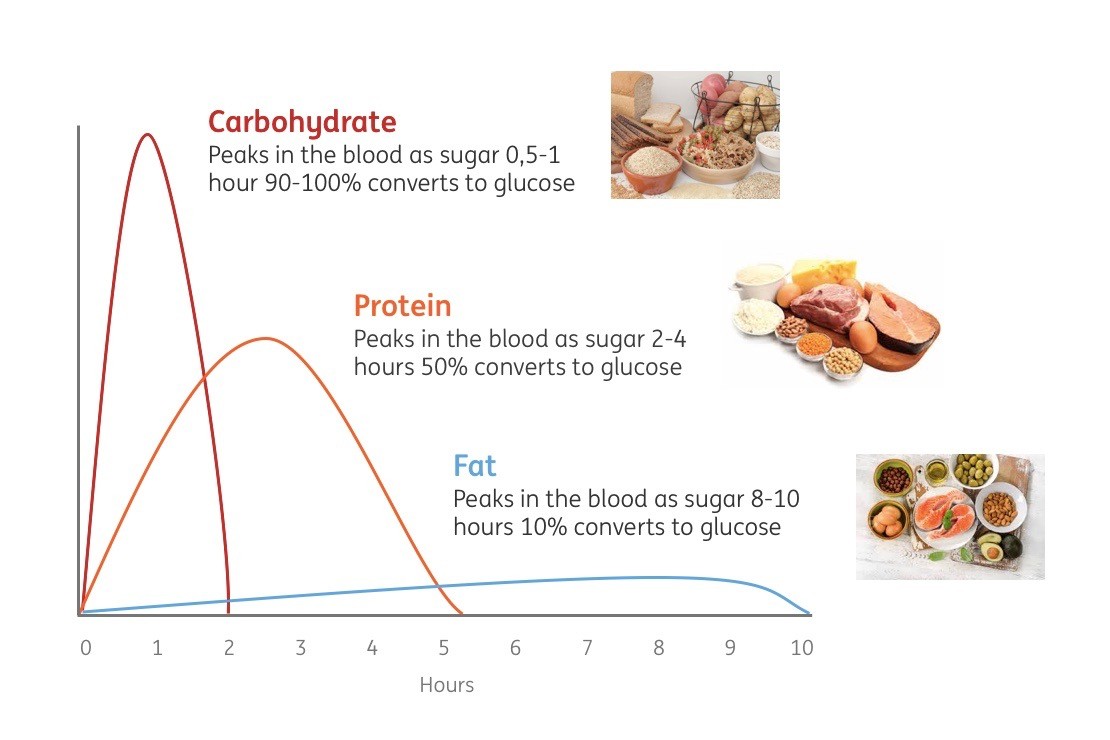
0 thoughts on “Macronutrients and blood sugar control”