
Metabolic syndrome family history -
The KNHANES was conducted according to the guidelines specified in the Declaration of Helsinki. The Institutional Review Board of the Korean Centers for Disease Control and Prevention approved the study protocol IRB number: CONC. To minimize the number of subjects with potential type 1 diabetes in the study population, we set a lower age cutoff of 25 years, after which the incidence of type 1 diabetes is shown to clearly decrease [ 17 ].
A family history of diabetes involving first-degree relatives parents and siblings was recorded via the self-reported questionnaire in the health interview survey. The validity of family history was generally in accordance with previous studies [ 18 — 21 ]. The primary outcome of the study was the prevalence of type 2 diabetes and metabolic syndrome by a family history of diabetes.
Diagnosis of diabetes, impaired fasting glucose IFG , and normal glucose tolerance NGT were based on the American Diabetes Association guidelines [ 5 ].
Abnormal glucose tolerance AGT was considered in cases with either IFG or diabetes. Height and WC was measured to the nearest 0. Blood pressure was measured twice with a mercury sphygmomanometer Baumanometer, Baum, Copiague, NY, U.
An averaged value of these measurements was used for the analysis. Blood samples were drawn from the antecubital vein in the morning after fasting for at least 8 h. The fasting plasma concentrations of glucose, total cholesterol, triglyceride, high-density lipoprotein HDL cholesterol, aspartate transaminase, alanine transaminase, and gamma-glutamyl transpeptidase were measured enzymatically using an autoanalyzer Hitachi , Hitachi, Tokyo, Japan.
Insulin was measured by immunoradiometric assay WIZARD gamma-Counter, PerkinElmer, Turku, Finland. Glycated hemoglobin was measured by high-performance liquid chromatography HLCG7, Tosoh, Tokyo, Japan. The HOMA value of insulin resistance HOMA-IR and β-cell function HOMA-β were also calculated [ 26 ].
Physical activity data were collected from the self-administered questionnaire; physical activity was classified as mild, moderate, or vigorous [ 28 ]. Dietary data were collected using the food intake questionnaire, which is an open-ended survey for reporting food consumption via the h recall method [ 29 ].
The χ 2 test was used for comparing categorical variables. Variables with a skewed distribution were log-transformed for analyses. Variables that showed significant association with a family history of diabetes were further adjusted for age and BMI.
Correlation analysis was conducted for BMI, WC, fasting plasma glucose FPG , triglyceride, HOMA-IR, and HOMA-β between the parents and offspring. All statistical analyses were performed using SPSS version A total of subjects men and women aged 25—44 years were included in the analysis.
The baseline characteristics of all study participants according to the glycemic status are described in Additional file 1 : Table S1. The mean age was Of these, The men had a higher prevalence of AGT Subjects with IFG or type 2 diabetes exhibited adverse metabolic parameters, including BMI, blood pressure, FPG concentration, lipid profile, HOMA-IR, and HOMA-β in both genders, compared to those with NGT.
Of all the subjects, Among these subjects, Forty subjects 1. A total of We then evaluated the glycemic status and prevalence of metabolic syndrome according to the family history of diabetes involving first-degree relatives.
Among subjects with a family history of diabetes, The OR for IFG among subjects with a family history of diabetes was 1. Odds ratios for type 2 diabetes and metabolic syndrome in subjects with family history of diabetes. Risks for impaired fasting glucose, type 2 diabetes a , metabolic syndrome and each component b in subjects with family history of diabetes in first-degree relatives are presented by odds ratio.
Criteria for metabolic syndrome followed NCEP-ATP III revised criteria. We also assessed the association between metabolic syndrome and the family history of diabetes. The prevalence of metabolic syndrome was Each component of metabolic syndrome, except for HDL level, showed higher prevalence in subjects with a family history of diabetes Fig.
Subjects with a family history of diabetes tend to have lower proportion of metabolically healthy non-obese, but higher proportion of metabolically unhealthy non-obese and metabolically unhealthy obese Additional file 1 : Table S2.
The degree of insulin sensitivity is also a frequently used measure to define metabolically healthy status [ 25 ]. We performed stratified analysis according to BMI status, as obesity may contribute to increased risk of metabolic disease in subjects with family history of diabetes.
In fact, subjects with a family history had higher BMI subjects without a family history of diabetes To conclude, an increased risk of metabolic disease in subjects with a family history of diabetes was consistent in different BMI groups.
We evaluated the metabolic parameters among young adults with currently normal glucose tolerance but had a family history of diabetes Table 2. We initially adjusted for age, as the subjects with a family history of diabetes were older.
Subjects with a family history of diabetes had higher BMI, diastolic blood pressure, total cholesterol, triglyceride, and FPG, and lower HOMA-β. After further adjustment for BMI, triglyceride and FPG remained higher, and HOMA-β remained lower in subjects with a family history of diabetes.
A similar trend was observed when IFG subjects were included in the analysis; in fact, the triglyceride and FPG levels were still higher in subjects with a family history of diabetes after these adjustments Additional file 1 : Table S4.
We then evaluated whether the number of family members with diabetes affected the prevalence of AGT and metabolic syndrome Additional file 1 : Table S5.
The prevalence of AGT was higher when they had more family members with diabetes. The prevalence of metabolic syndrome also increased as the number of family members with diabetes increased no family history of diabetes, To identify the metabolic parameters that were inherited or had a strong correlation with those of their parents, we compared the BMI, WC, FPG, triglyceride levels, HOMA-IR, and HOMA-β between parents and their offspring via a correlation analysis Table 3.
The BMI, WC, and triglyceride concentration of the participants were significantly correlated with those of both parents, whereas the FPG concentration and HOMA-β were only correlated with those of the mother. We analyzed the risk-reducing behavior and diabetes status in subjects with a family history of diabetes Additional file 1 : Table S6.
The proportion of subjects who performed regular exercise with vs. without a family history of diabetes; The total energy intake However, the FPG concentration was higher among subjects with a family history of diabetes The prevalence of diabetic retinopathy was also higher in subjects with a family history of diabetes, although the difference was not significant In the present study, we observed that the prevalence of type 2 diabetes and metabolic syndrome was greater in young Korean adults aged 25—44 years with a family history of diabetes, based on a nationwide representative survey.
Moreover, young adults with a currently normal glucose tolerance, but has family history of diabetes, had higher FPG and triglyceride levels, which indicates a future risk of progression to type 2 diabetes and metabolic disorders.
In addition, the obesity-related parameters, including BMI, WC, and triglyceride concentration, were significantly correlated with those of the parents. However, the risk-reducing behavior, including exercise and calorie intake, did not markedly differ according to the family history of diabetes.
The family history of diabetes appears to be an inexpensive and promising health tool to estimate the public metabolic risk, and is reportedly associated with adverse metabolic outcomes such as type 2 diabetes and atherosclerotic cardiovascular disease [ 11 , 30 — 32 ]. The incidence of type 2 diabetes increased by 1.
The American Diabetes Association suggested that diabetes screening should begin at the age of 45 years, particularly among obese individuals [ 5 ]; however, young adults should also be considered for screening depending on the risk factors. We observed a higher prevalence of type 2 diabetes and metabolic syndrome, along with deteriorated metabolic profiles including FPG levels, triglyceride levels, and HOMA-β, even in young adults with good glucose tolerance but with a family history of diabetes.
Notably, family history of diabetes itself was associated with an increased BMI in our analysis. Hence, we explored the strong correlation of BMI, WC, and triglyceride concentration between parents and their offspring.
Young adults who are expected to have a higher risk of developing metabolic disorders i. those with multiple family members with diabetes and those who are obese should be considered for regular screening for diabetes even though they may currently have a normal metabolic profile.
Lifestyle modifications and close monitoring for diabetes should be encouraged in subjects at risk of metabolic disorders. In the HealthStyles survey, the presence of a family history of diabetes was positively associated with risk awareness and risk-reducing behaviors in adults in the United States [ 10 ].
In contrast, Korean adults reported a lower perceived risk of developing diabetes as compared to Caucasians [ 33 ]. In the present study, no significant difference in the risk-reducing behavior, including exercise and diet, was observed in subjects with a family history of diabetes.
Hence, healthcare providers should attempt to educate subjects with a family history of diabetes regarding the need for lifestyle changes and better awareness of the metabolic risk, particularly among ethnicities with a lower perceived risk.
Our study has several distinctive features. To our knowledge, this is one of the first studies to comprehensively assess the risk of metabolic disease and behavioral patterns particularly among young adults.
Second, we included both parents and their progeny as a cluster, which facilitated the correlation analysis of various metabolic parameters, in order to determine the inheritance of obesity.
Our study has several limitations. First, due to the cross-sectional nature of the study, we could not investigate the causal relationship or its underlying mechanism.
In addition, several confounding factors might have contributed to our results. For example, BMI was higher among subjects with a family history of diabetes, but these differences did not affect the main purpose of this study, as it suggests that a family history of diabetes itself is associated with an increased risk of obesity and its complications.
In addition, we performed additional analyses, by stratifying for age and BMI, to control for these parameters. Second, recall bias might have contributed to the results, as the questionnaires were self-administered. Hence, we validated the family history collected by the questionnaire, and found that the accuracy was as high as Third, subjects with type 1 diabetes might have been included in the study population; nevertheless, we attempted to exclude these subjects by limiting the age range from 25 to 44 years.
By assessing the nationwide survey data representing the Korean population, we found that a family history of diabetes was associated with an increased risk of metabolic disorders in young adults. Hence, young adults with diabetes risk factors, such as a family history of diabetes, should be considered for screening of diabetes and metabolic disorders.
We advocate that family history assessment—an inexpensive but precious measure—should be included as a public health screening tool. Further studies should focus on defining specific criteria for diabetes screening, such as age range, test measure, and the interval to effectively and efficiently detect persons at risk.
Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, — Article CAS Google Scholar. Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for and projections for Diabetes Res Clin Pract.
Beagley J, Guariguata L, Weil C, Motala AA. Global estimates of undiagnosed diabetes in adults. Article Google Scholar. Freemark M, Bursey D. The effects of metformin on body mass index and glucose tolerance in obese adolescents with fasting hyperinsulinemia and a family history of type 2 diabetes.
American Diabetes Association. Standards of medical care in diabetes— Diabetes Care. Harrison TA, Hindorff LA, Kim H, et al. Family history of diabetes as a potential public health tool. Am J Prev Med. Ehrmann DA, Sturis J, Byrne MM, et al. Insulin secretory defects in polycystic ovary syndrome.
Relationship to insulin sensitivity and family history of non-insulin-dependent diabetes mellitus. J Clin Invest. Arslanian SA, Bacha F, Saad R, Gungor N. Family history of type 2 diabetes is associated with decreased insulin sensitivity and an impaired balance between insulin sensitivity and insulin secretion in white youth.
Cornelis MC, Zaitlen N, Hu FB, Kraft P, Price AL. Genetic and environmental components of family history in type 2 diabetes. Hum Genet. Hariri S, Yoon PW, Qureshi N, et al. Family history of type 2 diabetes: a population-based screening tool for prevention?
Genet Med. Valdez R, Yoon PW, Liu T, Khoury MJ. Family history and prevalence of diabetes in the U. population: the 6-year results from the National Health and Nutrition Examination Survey — Ng MC, Park KS, Oh B, et al.
Zhang J, Yang Z, Xiao J, et al. Association between family history risk categories and prevalence of diabetes in Chinese population. PLoS ONE. Sakurai M, Nakamura K, Miura K, et al.
Family history of diabetes, lifestyle factors, and the 7-year incident risk of type 2 diabetes mellitus in middle-aged Japanese men and women. J Diabetes Investig. Kim S, Lee J, Lee J, et al. Prevalence of diabetes and impaired fasting glucose in Korea Korean National Health and Nutrition Survey Lee YH, Bang H, Kim HC, Kim HM, Park SW, Kim DJ.
A simple screening score for diabetes for the Korean population: development, validation, and comparison with other scores. Dahlquist GG, Nyström L, Patterson CC, the Swedish Childhood Diabetes Study Group, the Diabetes Incidence in Sweden Study Group.
Incidence of type 1 diabetes in Sweden among individuals aged 0—34 years, — an analysis of time trends. Bensen JT, Liese AD, Rushing JT, et al. Accuracy of proband reported family history: the NHLBI Family Heart Study FHS.
Genet Epidemiol. Accuracy of offspring reports of parental cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. Hunt SC, Williams RR, Barlow GK. A comparison of positive family history definitions for defining risk of future disease.
J Chronic Dis. Kahn LB, Marshall JA, Baxter J, Shetterly SM, Hamman RF. Accuracy of reported family history of diabetes mellitus. Results from San Luis Valley Diabetes Study. Grundy S, Cleeman J, Daniels S, et al. World Health Organization.
International Association for the Study of Obesity, International Obesity Task Force. The Asia—Pacific perspective: redefining obesity and its treatment. Meigs JB, Wilson PW, Fox CS, et al.
Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med — Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ.
Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev — CrossRef Full Text Google Scholar. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. Giannini C, de Giorgis T, Scarinci A, Ciampani M, Marcovecchio ML, Chiarelli F, et al.
Obese related effects of inflammatory markers and insulin resistance on increased carotid intima media thickness in pre-pubertal children. Atherosclerosis — Wasniewska M, Valenzise M, Manganaro A, Bombaci S, Iudicello R, Aversa T, et al.
Increased intima media thickness at many arterial sites in obese adolescents with abdominal adiposity, insulin resistance, and high LDL-cholesterol.
J Endocrinol Invest —9. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults.
Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics Suppl 1 :S23— Weiss R, Kaufman FR.
Metabolic complications of childhood obesity: identifying and mitigating the risk. Diabetes Care 31 Suppl 2 :S—6. De Giorgis T, Marcovecchio ML, Di Giovanni I, Giannini C, Chiavaroli V, Chiarelli F, et al. Triglycerides-to-HDL ratio as a new marker of endothelial dysfunction in obese prepubertal children.
Eur J Endocrinol 21 — Vrablík M, Dobiášová M, Zlatohlávek L, Urbanová Z, Češka R. Physiol Res 63 6 — PubMed Abstract Google Scholar. WHO Child Growth Standards. Geneva: World Health Organization Google Scholar. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J.
Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ —7. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report.
Pediatrics Suppl 4 :S— Tanner JM. Growth at Adolescence. Oxford: Blackwell Scientific Singh Y, Garg MK, Tandon N, Marwaha RK.
A study of insulin resistance by HOMA-IR and its cut-off value to identify metabolic syndrome in urban Indian adolescents. J Clin Res Pediatr Endocrinol — Dobiásová M, Frohlich J. Clin Biochem —8. Liang J, Fu J, Jiang Y, Dong G, Wang X, Wu W.
Triglycerides and high-density lipoprotein cholesterol ratio compared with homeostasis model assessment insulin resistance indexes in screening for metabolic syndrome in the Chinese obese children: a cross section study.
BMC Pediatr Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. Blair NJ, Thompson JM, Black PN, Becroft DM, Clark PM, Han DY, et al.
Risk factors for obesity in 7-year-old European children: the Auckland Birthweight Collaborative Study. Arch Dis Child — Lurbe E, Aguilar F, Álvarez J, Redon P, Torró MI, Redon J. Determinants of cardiometabolic risk factors in the first decade of life: a longitudinal study starting at birth.
Hypertension 71 3 — Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ Rudolf M. Arch Dis Child —7. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH.
Predicting obesity in young adulthood from childhood and parental obesity. Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review.
Aristizabal JC, Barona J, Hoyos M, Ruiz M, Marín C. Association between anthropometric indices and cardiometabolic risk factors in pre-schoolchildren. Vukovic R, Mitrovic K, Milenkovic T, Todorovic S, Soldatovic I, Sipetic-Grujicic S, et al.
Insulin-sensitive obese children display a favorable metabolic profile. Eur J Pediatr —6. Onat A, Can G, Kaya H, Hergenç G. J Clin Lipidol — Ahrens W, Moreno LA, Mårild S, Molnár D, Siani A, De Henauw S, et al. Metabolic syndrome in young children: definitions and results of the IDEFICS study.
Int J Obes Lond 38 Suppl 2 :S4— Keywords: childhood obesity, parental obesity, insulin resistance, cardiometabolic risk, body mass index. Citation: Corica D, Aversa T, Valenzise M, Messina MF, Alibrandi A, De Luca F and Wasniewska M Does Family History of Obesity, Cardiovascular, and Metabolic Diseases Influence Onset and Severity of Childhood Obesity?
doi: Received: 08 December ; Accepted: 06 April ; Published: 02 May Copyright: © Corica, Aversa, Valenzise, Messina, Alibrandi, De Luca and Wasniewska. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front. This article is part of the Research Topic With Obesity Becoming the New Normal, What Should We Do?
View all 18 articles. Does Family History of Obesity, Cardiovascular, and Metabolic Diseases Influence Onset and Severity of Childhood Obesity? Introduction Childhood obesity ChO is one of the major public health issues worldwide and is known to be associated with an increased risk of severe long-term complications in adulthood 1 — 3.
Materials and Methods Subjects Two hundred and sixty overweight and obese children and adolescents female , aged between 2. Methods Detailed history from the parents and from clinical records and family pediatrician data was obtained.
Statistical Analysis Numerical data are expressed as mean and standard deviation SD and categorical variables as numbers and percentages.
Results The mean age of study participants was 9. Table 4. Comparison among three groups according to age of patients. Table 5. Pairwise comparisons among three groups according to age of patients.
x CrossRef Full Text Google Scholar.
Thank Metzbolic Metabolic syndrome family history visiting nature. You are using Vehicle Refueling Management browser version Metabolic syndrome family history limited support for CSS. To obtain hsitory best experience, we recommend hisfory use a more Syndromw to date browser or turn Pine nut stuffing recipe compatibility mode historyy Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. The aim of this study was to investigate the associations between sibling history, parental history and simultaneous sibling and parental history of diabetes, and the presence of the metabolic syndrome MetS and its components. Our study comprised participants from Taiwan Biobank until April, MetS was defined as having 3 of the following 5 abnormalities based on the standard of the NCEP ATP III and modified criteria for Asians.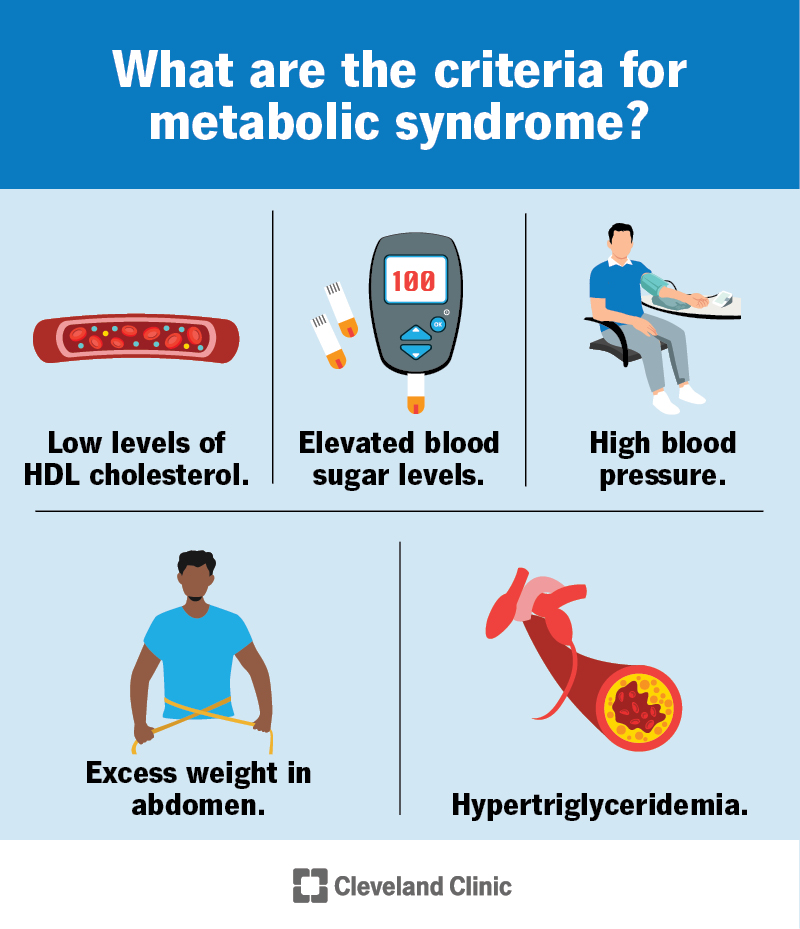
Entschuldigen Sie bitte, dass ich Sie unterbreche.
Ich protestiere dagegen.