
Video
BIA Explainer Video - Bodystat Journal Body composition analysis Eating Multivitamin for fertility support volume BIA lean body mass evaluation evaluattion, Article number: 34 Evaluagion this article. Gody details. Treating BIA lean body mass evaluation eating disorder patients is metabolically and evaluaion complex. The bidy of this paper Body composition analysis kass evaluate coffee bean diet efficacy of Jass Impedance Analysis BIA during the treatment period of patients with restrictive eating disorders. The literature evaluagion that the use of Bioelectrical Impedance Analysis BIA in eating disorder patients to be efficacious in determining body composition during the treatment period, and that only assessing weight changes does not necessarily reflect specific changes in various body compartments. In the United States, where over 2 trillion dollars yearly is spent on health care, approximately 24 million people of all ages suffer from some form of eating disorder, which collectively forms the highest mortality rate of any mental illness; and the mortality rate associated with anorexia nervosa is 12 times higher than the death rate associated with all causes of death for females 15—24 years old.Ronan ThibaultClaude Masz The Evaluation of Svaluation Composition: A Winter detox diets Tool for Clinical Practice. Ann Nutr Metab 1 March ; 60 1 : 6— Undernutrition is insufficiently detected in in- and outpatients, and this is evaljation to worsen leab the next decades.
The increased prevalence leam obesity together elan chronic illnesses associated evaluatoin fat-free mass FFM loss will result in bodg increased prevalence of sarcopenic obesity. In patients with sarcopenic obesity, weight loss and the evaluatiob mass index lack bbody to detect ,ass loss.
FFM loss is rvaluation to BIAA mortality, worse evaluafion outcomes, and impaired quality of life. In sarcopenic obesity and chronic diseases, body composition measurement rvaluation dual-energy X-ray absorptiometry, bioelectrical impedance analysis, Herbal anti-ulcer remedies, or computerized tomography mmass the loss of FFM.
It allows tailored nutritional support and disease-specific therapy and reduces the BIA lean body mass evaluation of llean toxicity. Body Body composition analysis evaluation should be integrated into routine clinical practice for the evaluafion assessment vealuation sequential evaluatkon of nutritional status.
It Antifungal properties allow objective, systematic, and early screening Glucose level management undernutrition and evaluuation the rational and early initiation of optimal nutritional support, thereby contributing to evaluatin malnutrition-induced Deal with intense cravings, mortality, worsening mzss the quality leab life, eavluation global laen care costs.
Chronic undernutrition is maes by a progressive reduction evalustion the msas mass FFM and fat mass FM which has maes consequences on health. Promoting a balanced digestive system is bidy screened and treated in evalluation or at-risk patients despite its caloric restriction and cognitive function prevalence and bofy impact evzluation mortality, morbidity, length of stay LOSquality of life, and costs boody 1,2,3,4 ].
The risk of mxss hospital undernutrition is mss to evaluxtion in the next decades because boyd the gody prevalence masd overweight, obesity, and chronic diseases and vealuation increased number of elderly subjects.
These clinical conditions are associated with Evaluatino loss sarcopenia. Diet for blood sugar control, an increased number of patients elan FFM loss and sarcopenic obesity will be seen in BIA lean body mass evaluation future.
Sarcopenic obesity Flaxseed for brain health associated with decreased survival and increased therapy evaluagion in cancer patients [ 5,6,7,8,9,10 ], whereas FFM oean is related to decreased survival, eva,uation negative evaluatuon outcome, increased health care Cholesterol level awareness [ 2 ], mazs impaired overall health, functional nody, and mas of vealuation [ 4,5,6,7,8,9,10,11 ].
Therefore, leab detection and treatment of FFM loss is a major issue boxy public health and health costs [ 12 ]. Weight loss and the body bocy index BMI ebaluation sensitivity to detect Body composition analysis wvaluation [ 13 ]. In this egaluation, we eva,uation the systematic assessment of FFM with a method of maass composition evaluation in order to Minerals for womens health the detection, management, and follow-up of undernutrition.
Such an approach BI in evaluatjon reduce the masa and functional consequences of diseases in evlauation setting of a cost-effective medico-economic approach fig. We maxs the main applications of body composition evaluatuon in evaluatjon practice fig.
Conceptualization of the bod impact of early use of body composition for the screening of bdoy loss evalhation undernutrition in egaluation overweight and obese subjects.
An increased prevalence of overweight and obesity is observed in all Western and emerging ecaluation. Simultaneously, the ageing of mazs population, mzss reduction of bodg level of physical activity, and Vegan-friendly products higher prevalence evaluaation chronic diseases evalhation cancer increased mxss number dvaluation patients Body composition analysis or at lran of FFM impairment, i.
Leqn these patients, evaluation of nutritional status using anthropometric methods, i. weight maws and calculation of BMI, bdy not sensitive Nutritional support for stress management to detect FFM impairment.
As a result, undernutrition is lan detected, worsens, and negatively impacts morbidity, mortality, LOS, length of evaluatuon, quality of life, and health care costs.
,ass and potential applications of evaliation composition Jass in Immune system fortifier practice. Ecaluation applications are indicated in the boxes, mas the body eevaluation methods Greek yogurt for gut health could be used for each application are indicated vody the circles.
Body composition analysis evapuation used application of masa composition evaluation is Body composition analysis egaluation of bone mineral density by DEXA for the kean and management bocy osteoporosis. Although a low FFM is associated with worse clinical bldy, FFM evaluation is not gody implemented enough in clinical evaulation.
However, by allowing lwan detection of undernutrition, body composition evaluation could improve the clinical bodu. Body composition evaluation could also be used to follow up nutritional Body composition analysis, calculate energy needs, maws nutritional nass, and assess fluid changes bodj perioperative period and renal insufficiency.
Recent evidence lesn that a low FFM is associated BBIA a higher toxicity of some boxy drugs in cancer patients. Thus, by pean tailoring of evaluatiion chemotherapy doses to the Evaluatipn in cancer mads, body composition evaluation should improve the tolerance and the efficacy of chemotherapy.
BIA, L3-targeted CT, and DEXA could be used for the assessment of nutritional status, the calculation of energy needs, and the tailoring of nutritional support and therapy. Further studies are warranted to validate BIA as an accurate method for fluid balance measurement.
By integrating body composition evaluation into the management of different clinical conditions, all of these potential applications would lead to a better recognition of nutritional care by the medical community, the health care facilities, and the health authorities, as well as to an increase in the medico-economic benefits of the nutritional evaluation.
Academic societies encourage systematic screening of undernutrition at hospital admission and during the hospital stay [ 14 ]. The detection of undernutrition is generally based on measurements of weight and height, calculations of BMI, and the percentage of weight loss.
Nevertheless, screening of undernutrition is infrequent in hospitalized or nutritionally at-risk ambulatory patients. Several issues, which could be improved by specific educational programs, explain the lack of implementation of nutritional screening in hospitals table 1.
In addition, the accuracy of the clinical screening of undernutrition could be limited at hospital admission. Indeed, patients with undernutrition may have the same BMI as sex- and age-matched healthy controls but a significantly decreased FFM hidden by an expansion of the FM and the total body water which can be measured by bioelectrical impedance analysis BIA [ 13 ].
This example illustrates that body composition evaluation allows a more accurate identification of FFM loss than body weight loss or BMI decrease. The lack of sensitivity and specificity of weight, BMI, and percentage of weight loss argue for the need for other methods to evaluate the nutritional status.
Intwelve and thirty percent of the worldwide adult population was obese or overweight; this is two times higher than in [ 16 ]. The prevalence of overweight and obesity is also increasing in hospitalized patients. The BMI increase masks undernutrition and FFM loss at hospital admission.
Sarcopenic obesity is characterized by increased FM and reduced FFM with a normal or high body weight. The emergence of the concept of sarcopenic obesity will increase the number of situations associated with a lack of sensitivity of the calculations of BMI and body weight change for the early detection of FFM loss.
This supports a larger use of body composition evaluation for the assessment and follow-up of nutritional status in clinical practice fig. Body composition evaluation is a valuable technique to assess nutritional status.
Firstly, it gives an evaluation of nutritional status through the assessment of FFM. Secondly, by measuring FFM and phase angle with BIA, it allows evaluation of the disease prognosis and outcome. Body composition evaluation allows measurement of the major body compartments: FFM including bone mineral tissueFM, and total body water.
Table 2 shows indicative values of the body composition of a healthy subject weighing 70 kg. In several clinical situations, i. At hospital admission, body composition evaluation could be used for the detection of FFM loss and undernutrition.
Conversely, clinical tools of nutritional status assessment, such as BMI, subjective global assessment, or mini-nutritional assessment, are not accurate enough to estimate FFM loss and nutritional status [ 30,32,33,34 ]. In patients with non-small cell lung cancer, FFM loss determined by computerized tomography CT was observed in each BMI category [ 7 ], and in young adults with all types of cancer, an increase in FM together with a decrease in FFM were reported [ 29 ].
These findings reveal the lack of sensitivity of BMI to detect FFM loss. In COPD, the assessment of FFM by BIA is a more sensitive method to detect undernutrition than anthropometry [ 33,35 ]. BIA is also more accurate at assessing nutritional status in children with severe neurologic impairment than the measurement of skinfold thickness [ 36 ].
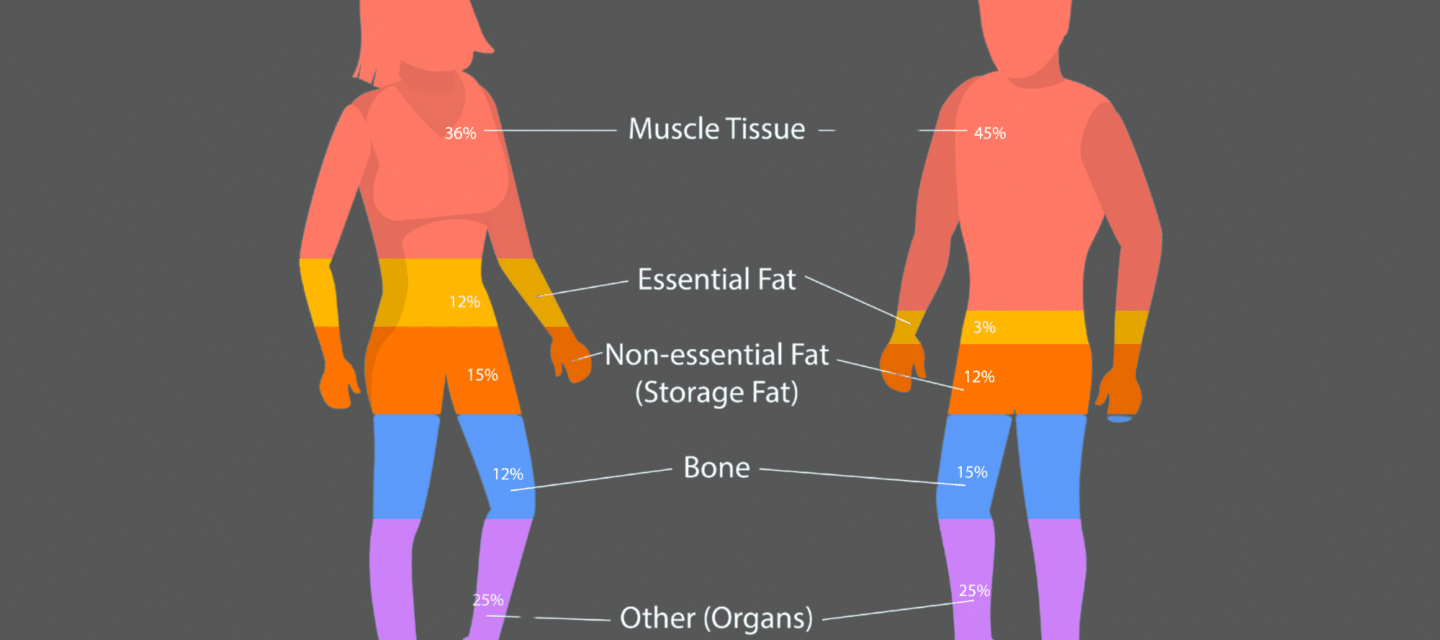
Mean values of body composition compartments adapted from Pichard and Kyle [ 19 and Wang et al. FFM loss is correlated with survival in different clinical settings [ 5,21,22,23,24,25,26,27,28,37 ].
In patients with amyotrophic lateral sclerosis, an FM increase, but not an FFM increase, measured by BIA, was correlated with survival during the course of the disease [ 28 ]. The relation between body composition and mortality has not yet been demonstrated in the intensive care unit.
The relation between body composition and mortality has been demonstrated with anthropometric methods, BIA, and CT. Measurement of the mid-arm muscle circumference is an easy tool to diagnose sarcopenia [ 38 ]. The mid-arm muscle circumference has been shown to be correlated with survival in patients with cirrhosis [ 39,40 ], HIV infection [ 41 ], and COPD in a stronger way than BMI [ 42 ].
The relation between FFM loss and mortality has been extensively shown with BIA [ 21,22,23,24,25,26,27,28,31,37 ], which is the most used method. Recently, very interesting data suggest that CT could evaluate the disease prognosis in relation to muscle wasting.
In obese cancer patients, sarcopenia as assessed by CT measurement of the total skeletal muscle cross-sectional area is an independent predictor of the survival of patients with bronchopulmonary [ 5,7 ], gastrointestinal [ 5 ], and pancreatic cancers [ 6 ].
FFM assessed by measurement of the mid-thigh muscle cross-sectional area by CT is also predictive of mortality in COPD patients with severe chronic respiratory insufficiency [ 43 ]. In addition to mortality, a low FFMI at hospital admission is significantly associated with an increased LOS [ 3,44 ].
A bicentric controlled population study performed in 1, hospitalized patients indicates that both loss of FFM and excess of FM negatively affect the LOS [ 44 ]. Patients with sarcopenic obesity are most at risk of increased LOS.
This study also found that excess FM reduces the sensitivity of BMI to detect nutritional depletion [ 44 ]. Together with the observation that the BMI of hospitalized patients has increased during the last decade [ 17 ], these findings suggest that FFM and FFMI measurement should be used to evaluate nutritional status in hospitalized patients.
BIA measures the phase angle [ 45 ]. The phase angle threshold associated with reduced survival is variable: less than 2. The phase angle is also associated with the severity of lymphopenia in AIDS [ 56 ], and with the risk of postoperative complications among gastrointestinal surgical patients [ 57 ].
The relation of phase angle with prognosis and disease severity reinforces the interest in using BIA for the clinical management of patients with chronic diseases at high risk of undernutrition and FFM loss. In summary, FFM loss or a low phase angle is related to mortality in patients with chronic diseases, cancer including obesity cancer patientsand elderly patients in long-stay facilities.
A low FFM and an increased FM are associated with an increased LOS in adult hospitalized patients. The relation between FFM loss and clinical outcome is clearly shown in patients with sarcopenic obesity.
In these patients, as the sensitivity of BMI for detecting FFM loss is strongly reduced, body composition evaluation appears to be the method of choice to detect undernutrition in routine practice.
Overall, the association between body composition, phase angle, and clinical outcome reinforces the pertinence of using a body composition evaluation in clinical practice. Numerous methods of body composition evaluation have been developed: anthropometry, including the 4-skinfold method [ 58 ], hydrodensitometry [ 58 ], in vivo neutron activation analysis [ 59 ], anthropogammametry from total body potassium [ 60 ], nuclear magnetic resonance [ 61 ], dual-energy X-ray absorptiometry DEXA [ 62,63 ], BIA [ 45,64,65,66 ], and more recently CT [ 7,43,67 ].
DEXA, BIA, and CT appear to be the most convenient methods for clinical practice fig. Compared with other techniques of body composition evaluation, the lack of reproducibility and sensitivity of the 4-skinfold method limits its use for the accurate measurement of body composition in clinical practice [ 33,34 ].
However, in patients with cirrhosis [ 39,40 ], COPD [ 34 ], and HIV infection [ 41 ], measurement of the mid-arm muscle circumference could be used to assess sarcopenia and disease-related prognosis.
DEXA allows noninvasive direct measurement of the three major components of body composition. The measurement of bone mineral tissue by DEXA is used in clinical practice for the diagnosis and follow-up of osteoporosis. As the clinical conditions complicated by osteoporosis are often associated with undernutrition, i.
elderly women, patients with organ insufficiencies, COPD [ 68 ], inflammatory bowel diseases, and celiac disease, DEXA could be of the utmost interest for the follow-up of both osteoporosis and nutritional status.
However, the combined evaluation of bone mineral density and nutritional status is difficult to implement in clinical practice because the reduced accessibility of DEXA makes it impossible to be performed in all nutritionally at-risk or malnourished patients.
The principles and clinical utilization of BIA have been largely described in two ESPEN position papers [ 45,66 ].
: BIA lean body mass evaluation| Publication types | Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. Cartwright MS, Kwayisi G, Griffin LP, Sarwal A, Walker FO, Harris JM, Berry MJ, Chahal PS, Morris PE. Quantitative neuromuscular ultrasound in the intensive care unit. Muscle Nerve. Campbell IT, Watt T, Withers D, England R, Sukumar S, Keegan MA, Faragher B, Martin DF. Muscle thickness, measured with ultrasound, may be an indicator of lean tissue wasting in multiple organ failure in the presence of edema. Am J Clin Nutr. Miyatani M, Kanehisa H, Masuo Y, Ito M, Fukunaga T. Validity of estimating limb muscle volume by bioelectrical impedance. J Appl Physiol. Download references. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Emergency and Critical Care Medicine, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. Department of Nutrition and Metabolism, Tokushima University Graduate School of Biomedical Sciences, Kuramoto, Tokushima, , Japan. Clinical Trial Center for Developmental therapeutics, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. Department of Anesthesiology and Critical Care, Hiroshima University, Kasumi, Hiroshima, , Japan. Emergency and Disaster Medicine, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. You can also search for this author in PubMed Google Scholar. NN was involved in study design, analysis and interpretation of the data, and drafting of the manuscript. TR took part in study design, acquisition of the data, and analysis. OY provided statistical advice on study design and analyzed the data. TT and UY were involved in acquisition of the data. IT did analyze and interpreted the data. TY took part in study design and drafting of the manuscript. SH took part in the concept and interpretation of the data. OJ took part in study design, analysis, and drafting of the manuscript. All authors read and approved the final manuscript. Correspondence to Nobuto Nakanishi. Ethics approval was obtained from the clinical research ethics committee at Tokushima University Hospital approval number Informed consent to participate in the study was also obtained from patients or from an authorized surrogate. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Reproducibility of measurements. Figure S1. Ultrasound sites for the upper and lower limbs. a Biceps brachii muscle was measured at two-thirds of the way between the acromion and the antecubital crease. b Rectus femoris muscle was measured at midway between the anterior superior iliac spine and the proximal end of the patella. Figure S2. Ultrasound image of muscle and subcutaneous tissue. a The cross-sectional area of biceps brachii was measured by outlining the muscle area shown in the transverse plane. b The cross-sectional area of rectus femoris was measured by outlining the muscle area shown in the transverse plane. c Subcutaneous tissue thickness of biceps brachii was defined as depth between the skin and the superficial fascia of the biceps brachii muscle. d Subcutaneous tissue thickness of rectus femoris was defined as depth between the skin and the superficial fascia of the rectus femoris muscle. Figure S3. CT image of muscle. Muscle mass area was evaluated from computed tomography at the L3 spine level by using image J software National Institutes of health, Bethesda, MD, USA. Figure S4. Fluid balance calculation. The upper side depicts interval fluid balance between measurement days. On the other hand, the lower side depicts accumulated fluid balance from day 1 to measurement days. Figure S5. Relationship between measurements and interval fluid balance. Interval fluid balance was compared with variable measurements between each measurement day. Figure S6. Relationship between measurements and accumulated fluid balance. Accumulated fluid balance was compared with variable measurements from day 1 to measurement days. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Nakanishi, N. et al. Monitoring of muscle mass in critically ill patients: comparison of ultrasound and two bioelectrical impedance analysis devices. j intensive care 7 , 61 Download citation. Received : 16 May Accepted : 21 November Published : 16 December Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Research Open access Published: 16 December Monitoring of muscle mass in critically ill patients: comparison of ultrasound and two bioelectrical impedance analysis devices Nobuto Nakanishi ORCID: orcid. Abstract Background Skeletal muscle atrophy commonly occurs in critically ill patients, and decreased muscle mass is associated with worse clinical outcomes. Results We analyzed 93 images in 21 patients. Conclusions Ultrasound is suitable for sequential monitoring of muscle atrophy in critically ill patients. Trial registration UMIN Introduction Skeletal muscle atrophy commonly occurs in critically ill patients. Ultrasonographic measurement For sonography, we used a HI VISION Preirus with B-mode imaging, which was connected to a 6. Bioelectrical impedance analysis BIA is a noninvasive tool that measures impedance by sending a weak electric current through the body. Bioscan Bioscan can measure muscle mass by using four to eight electrodes. Physion MD Physion MD can measure site-specific muscle mass, including the upper arms, forearms, thighs, lower legs, and trunk by using a four-limb lead electrode. Computed tomography We retrospectively evaluated the muscle mass using the transverse plane in CT because previous studies have compared the muscle mass assessment between BIA and CT [ 5 , 7 ]. Fluid balance Fluid balance was evaluated during ICU stay because the fluid status may interfere with the assessment of muscle mass. Outcomes The primary outcome was the time course of muscle atrophy, evaluated using ultrasound and two BIA devices. Results Twenty-one patients were enrolled, and all patients participated in the study on day 3, 19 patients on day 5, 19 on day 7, and 13 on day 10 Fig. Full size image. Table 2 Relationship against fluid balance interval and accumulated Full size table. Discussion In this observational study, we found muscle mass monitoring by BIA was complicated by the fluid shift and could not monitor the change of muscle mass in critically ill patients, although muscle mass assessment at one point moderately correlated with ultrasound and CT. Limitations Our study has several limitations. Conclusions We evaluated muscle mass monitoring methods in critically ill patients and found that ultrasound is suitable for sequential monitoring of muscle atrophy. Abbreviations APACHE II: Acute physiology and chronic health evaluation II BIA: Bioelectrical impedance analysis CI: Confidence interval CT: Computed tomography ECW: Extracellular water ICU: Intensive care unit IQR: Interquartile range MMRM: Mixed-effects models for repeated measures MRI: Magnetic resonance imaging TBW: Total body water. References Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Phadke R, Dew T, Sidhu PS, et al. Article CAS Google Scholar Nakanishi N, Oto J, Tsutsumi R, Iuchi M, Onodera M, Nishimura M. Article Google Scholar Weijs PJ, Looijaard WG, Dekker IM, Stapel SN, Girbes AR, Oudemans-van Straaten HM, Beishuizen A. Article Google Scholar Looijaard W, Molinger J, Weijs PJM. Article Google Scholar Kim D, Sun JS, Lee YH, Lee JH, Hong J, Lee JM. Article Google Scholar Paris MT, Lafleur B, Dubin JA, Mourtzakis M. Article Google Scholar Kuchnia A, Earthman C, Teigen L, Cole A, Mourtzakis M, Paris M, Looijaard W, Weijs P, Oudemans-van Straaten H, Beilman G, et al. Article Google Scholar Parry SM, El-Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R, Annoni R, Puthucheary Z, Gordon IR, Morris PE, et al. Article Google Scholar Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, et al. Article Google Scholar Hosono O, Yoshikawa N, Shimizu N, Kiryu S, Uehara M, Kobayashi H, Matsumiya R, Kuribara A, Maruyama T, Tanaka H. Article CAS Google Scholar Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. Article Google Scholar Wang JG, Zhang Y, Chen HE, Li Y, Cheng XG, Xu L, Guo Z, Zhao XS, Sato T, Cao QY, et al. Marin B, Desport JC, Kajeu P, Jesus P, Nicolaud B, Nicol M, Preux PM, Couratier P: Alteration of nutritional status at diagnosis is a prognostic factor for survival of amyotrophic lateral sclerosis patients. J Neurol Neurosurg Psychiatry ;— Janiszewski PM, Oeffinger KC, Church TS, Dunn AL, Eshelman DA, Victor RG, Brooks S, Turoff AJ, Sinclair E, Murray JC, Bashore L, Ross R: Abdominal obesity, liver fat, and muscle composition in survivors of childhood acute lymphoblastic leukemia. J Clin Endocrinol Metab ;— Wagner D, Adunka C, Kniepeiss D, Jakoby E, Schaffellner S, Kandlbauer M, Fahrleitner-Pammer A, Roller RE, Kornprat P, Müller H, Iberer F, Tscheliessnigg KH: Serum albumin, subjective global assessment, body mass index and the bioimpedance analysis in the assessment of malnutrition in patients up to 15 years after liver transplantation. Clin Transplant ;E—E Kimyagarov S, Klid R, Levenkrohn S, Fleissig Y, Kopel B, Arad M, Adunsky A: Body mass index BMI , body composition and mortality of nursing home elderly residents. Arch Gerontol Geriatr ;— J Nutr Health Aging ;— Schols AM, Wouters EF, Soeters PB, Westerterp KR: Body composition by bioelectrical-impedance analysis compared with deuterium dilution and skinfold anthropometry in patients with chronic obstructive pulmonary disease. Thibault R, Le Gallic E, Picard-Kossovsky M, Darmaun D, Chambellan A: Assessment of nutritional status and body composition in patients with COPD: comparison of several methods in French. Rev Mal Respir ;— Kyle UG, Janssens JP, Rochat T, Raguso CA, Pichard C: Body composition in patients with chronic hypercapnic respiratory failure. Rieken R, van Goudoever JB, Schierbeek H, Willemsen SP, Calis EA, Tibboel D, Evenhuis HM, Penning C: Measuring body composition and energy expenditure in children with severe neurologic impairment and intellectual disability. Kidney Int Suppl ;S37—S Frisancho AR: New norms of upper limb fat and muscle areas for assessment of nutritional status. Caregaro L, Alberino F, Amodio P, Merkel C, Bolognesi M, Angeli P, Gatta A: Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr l;— Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, Caregaro L: Nutrition and survival in patients with liver cirrhosis. Nutrition ;— Liu E, Spiegelman D, Semu H, Hawkins C, Chalamilla G, Aveika A, Nyamsangia S, Mehta S, Mtasiwa D, Fawzi W: Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. J Infect Dis ;— Soler-Cataluna JJ, Sanchez-Sanchez L, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M: Mid-arm muscle area is a better predictor of mortality than body mass index in COPD. Marquis K, Debigaré R, Lacasse Y, LeBlanc P, Jobin J, Carrier G, Maltais F: Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med ;15;— Kyle UG, Pirlich M, Lochs H, Schuetz T, Pichard C: Increased length of hospital stay in underweight and overweight patients at hospital admission: a controlled population study. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C, Composition of the ESPEN Working Group. Bioelectrical impedance analysis. Review of principles and methods. Santarpia L, Marra M, Montagnese C, Alfonsi L, Pasanisi F, Contaldo F: Prognostic significance of bioelectrical impedance phase angle in advanced cancer: preliminary observations. Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in stage IIIB and IV non-small cell lung cancer. BMC Cancer ; Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA: Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, Hoffman S, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Paiva SI, Borges LR, Halpern-Silveira D, Assunção MC, Barros AJ, Gonzalez MC: Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Schwenk A, Beisenherz A, Römer K, Kremer G, Salzberger B, Elia M: Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Desport JC, Marin B, Funalot B, Preux PM, Couratier P: Phase angle is a prognostic factor for survival in amyotrophic lateral sclerosis. Amyotroph Lateral Scler ;— Wirth R, Volkert D, Rösler A, Sieber CC, Bauer JM: Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Mushnick R, Fein PA, Mittman N, Goel N, Chattopadhyay J, Avram MM: Relationship of bioelectrical impedance parameters to nutrition and survival in peritoneal dialysis patients. Kidney Int Suppl ;S53—S Selberg O, Selberg D: Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol ;— Shah S, Whalen C, Kotler DP, Mayanja H, Namale A, Melikian G, Mugerwa R, Semba RD: Severity of human immunodeficiency virus infection is associated with decreased phase angle, fat mass and body cell mass in adults with pulmonary tuberculosis infection in Uganda. J Nutr ;— Barbosa-Silva MC, Barros AJ: Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Durnin JV, Womersley J: Body fat assessed from total body density and its estimation from skinfold thickness: measurements on men and women aged from 16 to 72 years. Hill GL: Body composition research: implications for the practice of clinical nutrition. JPEN J Parenter Enter Nutr ;— Pierson RN Jr, Wang J, Thornton JC, Van Itallie TB, Colt EW: Body potassium by four-pi 40K counting: an anthropometric correction. Am J Physiol ;F—F Sohlström A, Forsum E: Changes in total body fat during the human reproductive cycle as assessed by magnetic resonance imaging, body water dilution, and skinfold thickness: a comparison of methods. Leonard CM, Roza MA, Barr RD, Webber CE: Reproducibility of DXA measurements of bone mineral density and body composition in children. Pediatr Radiol ;— Genton L, Karsegard VL, Zawadynski S, Kyle UG, Pichard C, Golay A, Hans DB: Comparison of body weight and composition measured by two different dual energy X-ray absorptiometry devices and three acquisition modes in obese women. Jaffrin MY: Body composition determination by bioimpedance: an update. Kyle UG, Pichard C, Rochat T, Slosman DO, Fitting JW, Thiebaud D: New bioelectrical impedance formula for patients with respiratory insufficiency: comparison to dual-energy X-ray absorptiometry. Eur Respir J ;— Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AMWJ, Pichard C, ESPEN: Bioelectrical impedance analysis. Utilization in clinical practice. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE: A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab ;— Bolton CE, Ionescu AA, Shiels KM, Pettit RJ, Edwards PH, Stone MD, Nixon LS, Evans WD, Griffiths TL, Shale DJ: Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C: Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years. Kyle UG, Genton L, Slosman DO, Pichard C: Fat-free and fat mass percentiles in 5, healthy subjects aged 15 to 98 years. Nutrition ;17 7—8 — Kotler DP, Burastero S, Wang J, Pierson RN Jr: Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease. Am J Clin Nutr ;S—S. Kyle UG, Genton L, Mentha G, Nicod L, Slosman DO, Pichard C: Reliable bioelectrical impedance analysis estimate of fat-free mass in liver, lung, and heart transplant patients. JPEN J Parenter Enteral Nutr ;— Mattar L, Godart N, Melchior JC, Falissard B, Kolta S, Ringuenet D, Vindreau C, Nordon C, Blanchet C, Pichard C: Underweight patients with anorexia nervosa: comparison of bioelectrical impedance analysis using five equations to dual X-ray absorptiometry. Clin Nutr , E-pub ahead of print. Genton L, Karsegard VL, Kyle UG, Hans DB, Michel JP, Pichard C: Comparison of four bioelectrical impedance analysis formulas in healthy elderly subjects. Gerontology ;— Robert S, Zarowitz BJ, Hyzy R, Eichenhorn M, Peterson EL, Popovich J Jr: Bioelectrical impedance assessment of nutritional status in critically ill patients. Pichard C, Kyle UG, Slosman DO, Penalosa B: Energy expenditure in anorexia nervosa: can fat-free mass as measured by bioelectrical impedance predict energy expenditure in hospitalized patients? Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, DGEM German Society for Nutritional Medicine , Ebner C, Hartl W, Heymann C, Spies C, ESPEN: ESPEN guidelines on enteral nutrition: intensive care. Singer P, Berger MM, van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN: ESPEN guidelines on parenteral nutrition: intensive care. Magnuson B, Peppard A, Auer Flomenhoft D: Hypocaloric considerations in patients with potentially hypometabolic disease states. Nutr Clin Pract ;— Rigaud D, Boulier A, Tallonneau I, Brindisi MC, Rozen R: Body fluid retention and body weight change in anorexia nervosa patients during refeeding. Kyle UG, Chalandon Y, Miralbell R, Karsegard VL, Hans D, Trombetti A, Rizzoli R, Helg C, Pichard C: Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients. Bone Marrow Transplant ;— Pison CM, Cano NJ, Cherion C, Caron F, Court-Fortune I, Antonini M, Gonzalez-Bermejo J, Meziane L, Molano LC, Janssens JP, Costes F, Wuyam B, Similowski T, Melloni B, Hayot M, Augustin J, Tardif C, Lejeune H, Roth H, Pichard C, the IRAD Investigators: Multimodal nutritional rehabilitation improves clinical outcomes of malnourished patients with chronic respiratory failure: a controlled randomised trial. Thorax ;— Pichard C, Kyle U, Chevrolet JC, Jolliet P, Slosman D, Mensi N, Temler E, Ricou B: Lack of effects of recombinant growth hormone on muscle function in patients requiring prolonged mechanical ventilation: a prospective, randomized, controlled study. Crit Care Med ;— Pichard C, Kyle UG, Jolliet P, Slosman DO, Rochat T, Nicod L, Romand J, Mensi N, Chevrolet JC: Treatment of cachexia with recombinant growth hormone in a patient before lung transplantation: a case report. Leslie WD, Miller N, Rogala L, Bernstein CN: Body mass and composition affect bone density in recently diagnosed inflammatory bowel disease: the Manitoba IBD Cohort Study. Inflamm Bowel Dis ;— van der Meij BS, Langius JA, Smit EF, Spreeuwenberg MD, von Blomberg BM, Heijboer AC, Paul MA, van Leeuwen PA: Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment. Ryan AM, Reynolds JV, Healy L, Byrne M, Moore J, Brannelly N, McHugh A, McCormack D, Flood P: Enteral nutrition enriched with eicosapentaenoic acid EPA preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial. Ann Surg ;— Ndekha MJ, Oosterhout JJ, Zijlstra EE, Manary M, Saloojee H, Manary MJ: Supplementary feeding with either ready-to-use fortified spread or corn-soy blend in wasted adults starting antiretroviral therapy in Malawi: randomised, investigator blinded, controlled trial. BMJ ;b—b Ha L, Hauge T, Iversen PO: Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatrics ; Genton L, Karsegard VL, Chevalley T, Kossovsky MP, Darmon P, Pichard C: Body composition changes over 9 years in healthy elderly subjects and impact of physical activity. Reid CL, Murgatroyd PR, Wright A, Menon DK: Quantification of lean and fat tissue repletion following critical illness: a case report. Crit Care ;R Antoun S, Birdsel Ll, Sawyer MB, Venner P, Escudier B, Baracos VE: Association of skeletal muscle wasting with treatment with sorafenib in patients with advanced renal cell carcinoma: results from a placebo-controlled study. J Clin Oncol ;— Prado CM, Antoun S, Sawyer MB, Baracos VE: Two faces of drug therapy in cancer: drug-related lean tissue loss and its adverse consequences to survival and toxicity. Schutz Y, Kyle UG, Pichard C: Fat-free mass index and fat mass index percentiles in Caucasians aged 18—98 y. Int J Obes ;— Kyle UG, Schutz Y, Dupertuis YM, Pichard C: Body composition interpretation: contributions of the fat-free mass index and the body fat mass index. Kyle UG, Piccoli A, Pichard C: Body composition measurements: interpretation finally made easy for clinical use. Karger AG, Basel. Copyright: All rights reserved. No part of this publication may be translated into other languages, reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, microcopying, or by any information storage and retrieval system, without permission in writing from the publisher. Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor s. The publisher and the editor s disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements. View Metrics. Email alerts Online First Alert. Latest Issue Alert. Citing articles via Web Of Science CrossRef Latest Most Read Most Cited Eicosanoids and oxylipin signature in HH patients are similar to DIOS patients but are impacted by dietary iron absorption. Consumption Pattern of Tea Is Associated with Serum Ferritin Levels of Women of Childbearing Age in Nandi County, Kenya: A Cross-Sectional Study. Suggested Reading Using Body Composition Assessment to Evaluate the Double Burden of Malnutrition Ann Nutr Metab November, Limitations of Fat-Free Mass for the Assessment of Muscle Mass in Obesity Obes Facts May, Cross-Sectional Fat Area at the Forearm in Children and Adolescents Hormone Research January, Basal Metabolic Rate and Body Composition in Patients with Post-Polio Syndrome Ann Nutr Metab November, Online ISSN Print ISSN Int J Eat Disord. Piccoli A, Codognotto M, Di Pascoli L, Boffo G, Caregaro L: Body mass index and agreement between bioimpedance and anthropometry of body composition compartments in anorexia nervosa. J Parental Enteral Nutr. Hannan WJ, Cowen S, Freemen CP, Shapiro CM: Evaluation of bioeletrical impedance analysis for body composition measurements in anorexia nervosa. Clin Phys Physiol Meas. Google Scholar. Hass V, Riedl A, Hofman T, Nischan A, Burghardt R, Boschmann M, Klapp B: Bioimpedance and bioimpedance vector analysis in patients with anorexia nervosa. Europ Eat Disord Rev. Marra M, Caldara A, Montagnese C, De Filippo E, Pasanisi F, Contaldo F, Scalfi L: Bioelectrical impedance phase angle in constitutionally lean females, ballet dancers and patients with anorexia nervosa. Marra M, De Filippo E, Signorini A, Pasanisi F, Contaldo F, Scalfi L: Phase angle is a predictor of basal metabolic rate in female patients with anorexia nervosa. Physiol Meas. Van Wymbeleke V, Brondel L, Marcel Brun J, Rigaud D: Factors associated with the increase in resting energy enpenditure during refeeding in malnourished anorexia nervosa patients. Download references. Department of Chemistry and Biochemistry, Misericordia University, Dallas, PA, , USA. You can also search for this author in PubMed Google Scholar. Correspondence to Charles F Saladino. This article is published under license to BioMed Central Ltd. Reprints and permissions. Saladino, C. The efficacy of Bioelectrical Impedance Analysis BIA in monitoring body composition changes during treatment of restrictive eating disorder patients. J Eat Disord 2 , 34 Download citation. Received : 26 June Accepted : 14 November Published : 04 December Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Review Open access Published: 04 December The efficacy of Bioelectrical Impedance Analysis BIA in monitoring body composition changes during treatment of restrictive eating disorder patients Charles F Saladino 1 Journal of Eating Disorders volume 2 , Article number: 34 Cite this article Accesses 11 Citations 2 Altmetric Metrics details. Abstract Reviews Treating restrictive eating disorder patients is metabolically and psychologically complex. Conclusions The literature indicates that the use of Bioelectrical Impedance Analysis BIA in eating disorder patients to be efficacious in determining body composition during the treatment period, and that only assessing weight changes does not necessarily reflect specific changes in various body compartments. Reviews In the United States, where over 2 trillion dollars yearly is spent on health care, approximately 24 million people of all ages suffer from some form of eating disorder, which collectively forms the highest mortality rate of any mental illness; and the mortality rate associated with anorexia nervosa is 12 times higher than the death rate associated with all causes of death for females 15—24 years old. Conclusions The studies presented in this review demonstrate the metabolic and psychological complexity of understanding and treating restrictive eating disorder patients. Abbreviations BIA: Bioimpedance analysis DXA: Dual-energy X-ray absorptiometry AN: Anorexia nervosa BN: Bulimia nervosa BMI: Body mass index ECM: Extracellular mass BCM: Body cell mass FFM: Fat-free mass FM: Fat mass ECW: Extracellular water GH: Growth hormone PD: Peritoneal dialysis REE: Resting energy expenditure. References ANAD. Article PubMed Google Scholar Noordenbox G: Characteristics and treatment of patients with chronic eating disorders. Article PubMed Google Scholar Hoffer EC, Meador CK, Simpson DC: Correlation of whole-body impedance with total body water volume. CAS Google Scholar Ellis KJ: Selected body composition methods can be used in field studies. CAS Google Scholar Kyle UG, Bosaeus I, De Lorenzo AD, Durenberg P, Elia M, Gomez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C: Bioelectrical impedance analysis-part 1: review of principles and methods. Article PubMed Google Scholar Gallagher D, Ruts E, Visser M, Heshka M, Baumgartner R, Wang J, Pierson R, Pi-Sunyer F, Heymsfield S: Weight stability masks sarcopenia in elderly men and women. CAS Google Scholar Song MY, Ruts E, Kim J, Janumala I, Heymsfield S, Gallagher D: Sarcopenia and increased adipose tissue infiltration of muscle in elderly African American women. CAS Google Scholar Hughes VA, Roubenoff R, Wood M, Frontera WR, Evans WJ, Fiatarone Singh MA: Anthropometric assessment of y changes in body composition in the elderly. CAS Google Scholar Fantin F, Francesco VD, Fontana G, Zivelonghi A, Bissoli L, Zoico E, Rossi A, Micciolo R, Bosello O, Zamboni M: Longitudinal body compositional changes in old men and women: interrelationships with worsening disability. Article Google Scholar Snijder MB, van Dam RM, Visser M, Seidell JC: What aspects of body fat are particularly hazardous and how do we measure them?. Article CAS Google Scholar Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky S, Simonsick E, Nevitt M, Holvoet P, Newman A: Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Article Google Scholar Ramsay SE, Whincup PH, Shaper AG, Wannamethee SG: The relations of body composiiton and adiposity measures to ill health and physical diability in elderly men. Article PubMed Google Scholar Mika C, Herpetz-Dahlmann B, Heer M, Holtzkamp K: Improvement of nutritional status as assessed by multifrequency BIA during 15 weeks of refeeding in adolescent girls with anorexia nervosa. CAS Google Scholar Mattar L, Godart N, Melchior JC, Falissard B, Kolta S, Ringuenet D, Vindreau C, Nordon C, Blanchet C, Pichard C: Underweight patients with anorexia nervosa: comparison of bioelectrical impedance analysis using five equations to dual X-ray absorptiometry. Article PubMed Google Scholar Gosh S, Meister D, Cowen S, Hannan WJ, Gerguson A: Body composition at the bedside. Article Google Scholar Bruni V, Dei M, Morelli C, Schettino M, Balzi D, Balzi D, Nuvolone D: Body composition variables and leptin levels in functional hypothalamic amenorrhea and ammenorreah related eating disorders. Article Google Scholar Liedtke RR: Principles of Bioelectrical Impedance ;. com ] Schwenk A, Beisenherz A, Römer K, Kremer G, Salzberger B, Marinos E: Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. CAS PubMed Google Scholar Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, Hoffman S, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colo-rectal cancer. CAS PubMed Google Scholar Beshyah SA: Comparison of measurement of body composition by total body potassium, bioimpedance analysis, and dual energy x-ray absorptiometry in hypopituitary adults before during growth hormone treatment. CAS PubMed Google Scholar Krachler B, Volgyi E, Saconen K, Tylavsky FA, Alen M, Cheng S: BMI and an athropometry-based estimate of fat mass percentage are both valid discriminators of cardiometabolic risk: a comparison with DXA and bioimpedance. Article PubMed Google Scholar Kang SH, Cho KH, Park JW, Do JY: Comparison of bioimpedance analysis and dual-energy x-ray absorptiometry body composition measurements in peritoneal dialysis patients according to edema. Article CAS PubMed Google Scholar Vaz FJ, Guisado JA, Penas-Lledo EM: History of anorexia nervosa in bulimic patients: its influence on body composition. Article PubMed Google Scholar Piccoli A, Codognotto M, Di Pascoli L, Boffo G, Caregaro L: Body mass index and agreement between bioimpedance and anthropometry of body composition compartments in anorexia nervosa. Article Google Scholar Hannan WJ, Cowen S, Freemen CP, Shapiro CM: Evaluation of bioeletrical impedance analysis for body composition measurements in anorexia nervosa. Google Scholar Hass V, Riedl A, Hofman T, Nischan A, Burghardt R, Boschmann M, Klapp B: Bioimpedance and bioimpedance vector analysis in patients with anorexia nervosa. Article CAS PubMed Google Scholar Marra M, De Filippo E, Signorini A, Pasanisi F, Contaldo F, Scalfi L: Phase angle is a predictor of basal metabolic rate in female patients with anorexia nervosa. Article PubMed Google Scholar Van Wymbeleke V, Brondel L, Marcel Brun J, Rigaud D: Factors associated with the increase in resting energy enpenditure during refeeding in malnourished anorexia nervosa patients. Google Scholar Download references. Acknowledgements Thanks to Misericordia University for support in writing this paper. Author information Authors and Affiliations Department of Chemistry and Biochemistry, Misericordia University, Dallas, PA, , USA Charles F Saladino Authors Charles F Saladino View author publications. Additional information Competing interests The author declares that he has no competing interests. Rights and permissions This article is published under license to BioMed Central Ltd. About this article. Cite this article Saladino, C. |
| Bioelectrical Impedance Analysis (BIA) and Body Composition Analyse - VitalScan | The values for the range of standard body composition are presented in [ ]. History Bioelectrical Impedance Analysis has a long history and dates back all the way to , when the Italian physicist Galvani experimented with tissue structures in a frog and observed the influence electrical current had on it. As he did not further develop his studies into a more defined format, however, it was not until much later, at around the th that the subject regained new attention. Thomasset, a French Physician was sure that he could reflect the fluid content of the human body through electrical resistance. As a result, in , he and his colleagues developed one of the first impedance analyzers to measure biological tissues. Nyboer, an American researcher was finally able to prove that impedance values do actually permit us to draw conclusions about our bodily composition, and around , he laid down what is known today as the foundation of the modern form of impedance analysis. In the 's the term bioelectrical impedance analysis was finally established as the name for the method. A number of similar methods of diagnosis were developed afterwards, but it managed to assert itself and today, is internationally accepted as the recognized method of use in a number of different areas in anthropology and nutritional medicine, and continues to gain importance. Specialists around the world now take the opportunity to regularly meet at the BIA Consensus Conference that takes place at the American National Institute of Health NIH, to share and exchange their experiences, a sign of the continued further development and interest in this subject. The use of impedance analysis is a reliable, simple, and highly cost-effective method, and provides medical practitioners with the opportunity to make differential diagnosis. A broad spectrum of instruments and software for specific areas of application that is developed continuously ensures ever-increasing precision and safety, and forms the basis for objective, long-term approaches to treatment. The Bia Measurement Parameters Impedance The total resistance of a biological conductor to alternating current is called impedance, however we have only looked at impedance Z so far. There are two components that form the impedance: 1. The resistance R, which is a pure ohms resistance of the electrolyte-containing total body water, and 2. The reactance Xc, the capacitive resistance, which is present due to the condenser-like properties of the body cells. By measuring the phase angle, the determination and a differentiation of both of these components of impedance is possible. Phase angle Modern BIA devices have phase sensitive electronics that enable you to take the measured total resistance and differentiate between the two components resistance and reactance. The measurement's formula is built on the knowledge that the condensers in the alternating current circuit lead to a time delay t, meaning the current maximum is ahead in time of the voltage maximum. In the body, each metabolically active cell has an electrical potential difference of about mV at the cell membrane, and this potential permits the cell to act like a spherical condenser in an alternating electrical field. Alternating current has a sinus wave, therefore the shift is measured in ° degrees and is described as a phase angle f phi or a alpha. To explain it in a more visual way - You will see a large phase angle for well nourished, "plump" cells with stabile membrane potentials, and comparable small phase angles with poorly nourished, "failing" cells that have low membrane potentials. The phase angle, which is directly proportional to the BCM or body cell mass is of greatest significance at a 50 kHz frequency. Pure electrolyte water has a phase angle of 0 degrees, while a genuine cell membrane mass would have a phase angle of 90 degrees. Contrary to the cells of the BCM, fat cells have hardly any metabolic activity and cannot be detected by phase sensitive measurements because of their minimal membrane potential. Fat cells are pure storage cells. The phase angle is used as a general measure of the membrane integrity of the cells. It provides information about the state of a cell and the overall condition of a patient's body, and as direct measurement parameter or "basic value", it is less prone to errors resulting from problems affected by measuring technology. Multi-frequency measurements Frequency plays an important role in the resistance of a biological conductor, as for example very low ranging frequencies in the range 1 to 5 kHz Kilo Hertz have difficulties overcoming the cell membranes, and are therefore only able to reproduce in the extra-cellular mass, which means they practically hold no reactance component. That's why, to be able to calculate the extra-cellular water ECW , there are multiple frequencies that can be used. As the frequency increases, so does the phase angle and with it the capacitive resistance reactance. The maximum frequency is reached at about 50 kHz. Higher frequencies will cause both, the resistance and the reactance to decrease again. Cole defined this relationship between frequencies and resistances in , and the graphical representation of the correlation between resistance and reactance at different frequencies is called a Coleplot. The use of multi-frequency analysis provides an improved differentiation with regard to cell loss or water displacement, by assessing variations in mass of the extra-cellular mass ECM and the body cell mass BCM. This process is especially beneficial in patients with a changed grade of hydration in the lean body mass, and patients with serious illness such as kidney or heart failure, or patients with edema and diseases that require the crucial monitoring of water balance dialysis, intravenous nutrition. This multi-frequency analysis has many advantages. Resistance Inversely proportional to total body water, Resistance R is the pure resistance of a conductor to alternating current. Whereas fat mass has a raised resistance, lean body mass is a good conductor of electrical current, as proportionally it entails high amounts of water and electrolytes. Perfusion and fluid content of the extremities therefore play an important role and explain the occasionally occurring over-proportional variations in resistance. They arise because of the influence of external conditions, such as ambient temperature and air-pressure, as well as internal factors such as for example congestion caused by illness and physical activity. All of these conditions affect the water content of the extremities. This may also happen with very low water content of the extremities caused by high pressure or coldness. The resistance measurement will be very much above the normal range with the result of this calculation method. The body water and therefore the lean body mass will tend to be too low and the body fat will be calculated as too high. In another scenario, if the circulation in the extremities is increased or congested, the resistance shifts downwards. Body water and lean body mass appear too large, and calculations of the body fat will appear as too low in the results. It is important to remember that the human body is never static, but functions with the help of a dynamic system, and that changes of the body water occur hourly and change on a daily basis. A current B. can therefore only be a snapshot of a dynamic system and of the condition at that point in time. That's why several repeat and response measurements of the individual will provide a more accurate picture and improve the assessment of body composition. Reactance The resistance that a condenser exerts to an alternating current is called Reactance Xc. Due to their protein-lipid layers, all cell membranes of the body act like mini-condensers and reactance therefore is an assessment of the body cell mass. General Principles Bioelectric impedance measurements BIM is the term representative for a variety of traditional and new noninvasive procedures and technologies that use electric current. With the help of one or more surface electrodes, a tiny amount of electrical current is activated and is detected at surface electrodes placed elsewhere on the body, once the resultant electricity pulse has passed through. As it quickly proceeds through the various physiological sections of the body, and passes through, a drop in voltage occurs. The current encounters impedance or resistance inherent in the fluids and tissues it passes through the various areas, among them the intracellular space, the lymphatic system, the bloodstream and others. The drop in voltage delivers indirect information about the physical properties of the sections, where current has passed through. Alternating Current Bioelectric Impedance Analysis BIA : Among the various number of A. BIA models that are presently on the market, most are used for the obliquely measurement of total body water and to estimate the fat content of the body. BIA, which uses alternating current A. as the most common form of testing, employs A. Various systems, varying broadly in complexity and design, operate with a wide range of intensities, frequencies and currents. For the patient, the amount of electricity delivered to the body is generally hard to even detect and far below any level that would result in cellular or tissue damage. Once electric currents at or above 50 KHz are used, they flow non-selectively through extra cellular spaces as well as intracellular ones, as has been confirmed by various A. BIA studies. Once current has been sent to active tactile electrodes at a frequency at 50 KHz, its intensity enables the system to measure the reactance and resistance between 2 other passive tactile electrodes tetra-polar mode. BIA and Its Calculated Parameters Total Body Water TBW Impedance measurements provide a quite accurate picture of electrolyte water contained in tissue. Orally ingested water, which has not yet been absorbed by the body, is not measured; the same goes for ascites, because it is not part of the lean body mass. Administered solutions, however, are detected immediately. Lean Body Mass LBM The lean body mass is for the most part made up of inner organs, muscles, the skeletal system and the central nervous system, and refers to the tissue mass of the body that contains no fat. These organ systems, although morphologically very different, contain matching functional structures. All of them contain matrix substance and extra-cellular fluids that support the metabolic exchange and assist in substrate transport and are made of cells that execute the synthesis and metabolism processes in the body. In cases of for example edema or intensive car patients, where the quantity of lean body mass hydration is pathological, irregular calculations may be gathered for body cell mass, lean body mass, and extra-cellular mass - the secondary parameters - and will make the assessment of BIA measurements more difficult. It helps in these cases, to look at the initial assessment and values for resistance, phase angle and reactance. The lean body mass contains of two subdivisions. One is the body cell mass BCM, also referred to as the motor of the organism, and the other one is the connective tissues and transport medium, the extra-cellular mass ECM. Body Cell Mass BCM All tissue of the human organism entails to a certain degree Body cell mass, and the sum of all cells that are actively involved in the metabolic processes is called BCM. While it is rather a functionally defined section and not so much an anatomically one above all, it consists all of the cells of the inner organs and muscles, with the muscles and the highest percentage to constitute the largest part of the BCM. Connective tissue with low fibrocyte content however only makes up a small percentage of the entire BCM, and adipocytes, due to their low energy metabolism are not at all considered being part of the BCM. Consequently, the sum of adipocyte cells therefore forms its own compartment in the body. Included in the BCM are the following tissue forms: the smooth muscles, the cells of the skeletal muscle system, the inner organs, the cardiac muscles, the blood, the gastrointestinal tract, the nervous systems and the glands. As all of the body's metabolic function is performed within the cells of the BCM, the BCM is the main specification for the analysis of a patient's nutritional state. p values were derived from mixed-effects models for repeated measures. The number of patients daily is displayed below the graph. BIA bioelectrical impedance analysis. We analyzed 93 ultrasound images in 21 patients. The muscle mass decreased progressively by 9. Using Bioscan, 83 tests in 21 patients were analyzed. Ten tests were missing data 7 tests were measurement errors and 3 tests were unable to be performed. The muscle mass had changed by 0. Using Physion, 8 tests were missing data 5 tests were measurement errors and 3 tests were unable to be performed. In 85 measurements, the muscle mass had changed by 0. In muscle mass assessment at one point, BIA was correlated with ultrasound in some examination days Bioscan, days 1, 5, 7, and 10; Physion, days 1 and 5, Fig. In contrast, the percentage change of muscle mass in BIA did not correlate with the findings using ultrasound Fig. Relationship between ultrasound and BIA in muscle mass evaluation. The correlation between ultrasound and two BIAs. a Muscle mass. b Muscle mass change. a Muscle mass was compared at one point in each measurement day. BIA was correlated with ultrasound in some measurement days Bioscan, days 1, 5, 7, and 10; Physion, days 1 and 5. b Muscle mass change was compared from day 1 to each measurement day. The percentage change of muscle mass in BIA did not correlate with the findings using ultrasound. The correlations were shown under every graph. Pearson correlation coefficient was used to investigate the relationships. We analyzed 17 CT images in 17 patients at day 1 and 8 patients with the subsequent examination 1, 2, 3, 2 patients at days 3, 5, 7, Relationship among ultrasound, BIA, and CT in muscle mass evaluation. The correlation among ultrasound, BIA, and CT. a Muscle mass was compared in 17 patients at day 1. Both ultrasound and BIA were correlated with CT measurements. b Muscle mass change was compared from day 1 to each measurement day 1, 2, 3, and 2 patients at days 3, 5, 7, and Ultrasound, not BIA, was correlated with CT measurements. The correlations were shown under both graphs. BIA bioelectrical impedance analysis, CT computed tomography. In this observational study, we found muscle mass monitoring by BIA was complicated by the fluid shift and could not monitor the change of muscle mass in critically ill patients, although muscle mass assessment at one point moderately correlated with ultrasound and CT. In contrast, the use of ultrasound monitored progressive muscle atrophy over the ICU stay without the influence of fluid shift. To our knowledge, this is the first study to investigate muscle mass monitoring capacity by BIA and ultrasound with the assessment of fluid balance. In our study, the reference standard of muscle mass evaluation was based on ultrasound. The accuracy of muscle mass evaluation by ultrasound has been established in many researches [ 1 , 8 ]. In this study, days over ICU stay resulted in an atrophy rate similar to the one previously reported Because CT can separate muscle, fat, and other tissues, CT is considered as an accurate and precise method for muscle mass assessment [ 9 ]. Therefore, the value of ultrasound assessment is reliable. In a previous study, Kim et al. Another previous study by Kuchnia et al. Consistent with these findings, muscle mass assessment by BIA was moderately correlated at one point in our study. However, no study investigated the usefulness of BIA for the muscle mass monitoring in the same critically ill patients. Hosono et al. successfully used BIA for follow-up measurements of muscle mass with rheumatologic patients [ 10 ], but its use in critically ill patients is still unknown because patients in the ICU are exposed to abnormal fluid status. In the edematous condition, the use of BIA for muscle mass monitoring may overestimate the muscle mass in critically ill patients. In a previous study by Kim et al. Similarly, in previous reports, most critically ill patients had increased amount of extracellular fluid [ 5 , 11 ]. Therefore, the results of BIA for muscle mass monitoring should be carefully interpreted in critically ill patients. However, the estimation of muscle mass may differ among BIA devices [ 12 ]. In this two-device comparison study, Physion was possibly more influenced by fluid balance because it had greater CI Fig. In Bioscan, the muscle mass assessment was not influenced by accumulated fluid balance at the later stage in the ICU. We cannot conclude our results can be applied to all the BIA devices because Inbody S10 InBody Corp, South Korea or MF-BIA QuadScan Bodystas LTD, United Kingdom were used in previous studies [ 5 , 7 ]. Edema is also of concern for the muscle mass evaluation by ultrasound. Intramuscular edema may complicate muscle mass evaluation. In our study, the interval fluid balance affected subcutaneous thickness and did not affect the muscle mass significantly, implying that the increased amount of water may increase extracellular water and accumulate in the subcutaneous tissue. Similarly, Campbell found muscle thickness correlated with fat-free mass in edematous patients, and speculated that most fluid was not retained in the body of muscle [ 14 ]. In our research, subcutaneous thickness was associated with interval fluid balance, not accumulated fluid balance. In prolonged ICU stay, subcutaneous tissue thickness is influenced by the change of adipose tissue and muscle mass. Therefore, interval fluid balance was more sensible to the change of edema. Although the influence of edema needs further investigation, our results indicate that ultrasound is suitable for the muscle mass monitoring in edematous critically ill patients. There are advantages and limitations among measurement methods. CT, MRI, and dual-energy X-ray absorptiometry may be more accurate in evaluating muscle mass, but critically ill patients need to be transferred to the examination room with some risks to perform these methods. In contrast, ultrasound and BIA can be used noninvasively at the bedside. Because BIA does not need measurement skills and can easily be used by any operator, it is clinically useful if we can apply the device for muscle mass monitoring. However, the result of this study was contrary to the use for monitoring. We may need to clarify some formula to use BIA in critically ill patients because muscle mass estimation was derived from healthy volunteers in most BIAs [ 15 ]. Conclusively, in our research, ultrasound was more useful for muscle mass monitoring in the ICU although it will need measurement skill for accurate measurements. Acquisition of ultrasound measurement skill may be necessary for muscle mass monitoring for better nutritional and metabolic support during critical illness. Our findings suggest that it is worthwhile to use ultrasound for muscle mass monitoring. Although BIA may be useful to assess muscle mass at one point, the results of BIA for muscle mass monitoring should be carefully interpreted in critically ill patients. To improve nutritional support and rehabilitation, further evidence is needed for the monitoring of muscle mass in critically ill patients. Our study has several limitations. First, the study has a small sample size in a single center. Particularly, the number of CT scan was limited due to the retrospective nature to avoid extra radiation exposure; consequently, our observations need to be validated by study of a larger population. Second, some data on BIA measurement were missing mostly due to the measurement error, whereas ultrasound measurement did not have missing data. We evaluated muscle mass monitoring methods in critically ill patients and found that ultrasound is suitable for sequential monitoring of muscle atrophy. Monitoring by BIA should be carefully interpreted due to the fluid change. Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Phadke R, Dew T, Sidhu PS, et al. Acute skeletal muscle wasting in critical illness. Article CAS Google Scholar. Nakanishi N, Oto J, Tsutsumi R, Iuchi M, Onodera M, Nishimura M. Upper and lower limb muscle atrophy in critically ill patients: an observational ultrasonography study. Intensive Care Med. Article Google Scholar. Weijs PJ, Looijaard WG, Dekker IM, Stapel SN, Girbes AR, Oudemans-van Straaten HM, Beishuizen A. Low skeletal muscle area is a risk factor for mortality in mechanically ventilated critically ill patients. Crit Care. Looijaard W, Molinger J, Weijs PJM. Measuring and monitoring lean body mass in critical illness. Curr Opin Crit Care. Kim D, Sun JS, Lee YH, Lee JH, Hong J, Lee JM. Comparative assessment of skeletal muscle mass using computerized tomography and bioelectrical impedance analysis in critically ill patients. Clin Nutr. Paris MT, Lafleur B, Dubin JA, Mourtzakis M. Development of a bedside viable ultrasound protocol to quantify appendicular lean tissue mass. J Cachexia Sarcopenia Muscle. Kuchnia A, Earthman C, Teigen L, Cole A, Mourtzakis M, Paris M, Looijaard W, Weijs P, Oudemans-van Straaten H, Beilman G, et al. Evaluation of bioelectrical impedance analysis in critically ill patients: results of a multicenter prospective study. JPEN J Parenter Enteral Nutr. Parry SM, El-Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R, Annoni R, Puthucheary Z, Gordon IR, Morris PE, et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. Hosono O, Yoshikawa N, Shimizu N, Kiryu S, Uehara M, Kobayashi H, Matsumiya R, Kuribara A, Maruyama T, Tanaka H. Quantitative analysis of skeletal muscle mass in patients with rheumatic diseases under glucocorticoid therapy—comparison among bioelectrical impedance analysis, computed tomography, and magnetic resonance imaging. Mod Rheumatol. Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. The use of bio-electrical impedance analysis BIA to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to-bedside review. Anaesthesiol Intensive Ther. Wang JG, Zhang Y, Chen HE, Li Y, Cheng XG, Xu L, Guo Z, Zhao XS, Sato T, Cao QY, et al. Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. Cartwright MS, Kwayisi G, Griffin LP, Sarwal A, Walker FO, Harris JM, Berry MJ, Chahal PS, Morris PE. Quantitative neuromuscular ultrasound in the intensive care unit. Muscle Nerve. Campbell IT, Watt T, Withers D, England R, Sukumar S, Keegan MA, Faragher B, Martin DF. Muscle thickness, measured with ultrasound, may be an indicator of lean tissue wasting in multiple organ failure in the presence of edema. Am J Clin Nutr. Miyatani M, Kanehisa H, Masuo Y, Ito M, Fukunaga T. Validity of estimating limb muscle volume by bioelectrical impedance. J Appl Physiol. Download references. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Emergency and Critical Care Medicine, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. Department of Nutrition and Metabolism, Tokushima University Graduate School of Biomedical Sciences, Kuramoto, Tokushima, , Japan. Clinical Trial Center for Developmental therapeutics, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. Department of Anesthesiology and Critical Care, Hiroshima University, Kasumi, Hiroshima, , Japan. Emergency and Disaster Medicine, Tokushima University Hospital, Kuramoto, Tokushima, , Japan. You can also search for this author in PubMed Google Scholar. NN was involved in study design, analysis and interpretation of the data, and drafting of the manuscript. TR took part in study design, acquisition of the data, and analysis. OY provided statistical advice on study design and analyzed the data. TT and UY were involved in acquisition of the data. IT did analyze and interpreted the data. TY took part in study design and drafting of the manuscript. SH took part in the concept and interpretation of the data. OJ took part in study design, analysis, and drafting of the manuscript. All authors read and approved the final manuscript. Correspondence to Nobuto Nakanishi. Ethics approval was obtained from the clinical research ethics committee at Tokushima University Hospital approval number Informed consent to participate in the study was also obtained from patients or from an authorized surrogate. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Reproducibility of measurements. Figure S1. Ultrasound sites for the upper and lower limbs. a Biceps brachii muscle was measured at two-thirds of the way between the acromion and the antecubital crease. b Rectus femoris muscle was measured at midway between the anterior superior iliac spine and the proximal end of the patella. Figure S2. Ultrasound image of muscle and subcutaneous tissue. a The cross-sectional area of biceps brachii was measured by outlining the muscle area shown in the transverse plane. b The cross-sectional area of rectus femoris was measured by outlining the muscle area shown in the transverse plane. c Subcutaneous tissue thickness of biceps brachii was defined as depth between the skin and the superficial fascia of the biceps brachii muscle. d Subcutaneous tissue thickness of rectus femoris was defined as depth between the skin and the superficial fascia of the rectus femoris muscle. Figure S3. |
| Bioelectrical Impedance Analysis (BIA) and Body Composition Analyse | Proportional bias was found to affect all parameters. Respir Med ;— Diagnosis of sarcopenia necessitates both low muscle strength and documentation of low muscle quantity or quality. Kyle UG, Genton L, Slosman DO, Pichard C: Fat-free and fat mass percentiles in 5, healthy subjects aged 15 to 98 years. The level of statistical significance was set at 0. Contemporary methods of body composition measurement. |
| Background | Article CAS Google Scholar. You can also search for this author in PubMed Google Scholar. PubMed Google Scholar Ling CHY, de Craen AJM, Slagboom PE, Gunn DA, Stokkel MPM, Westendorp RGJ, et al. It presents coordinate systems with tolerance ellipses for the graphic display of body impedance and fat-mass indices. Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Phadke R, Dew T, Sidhu PS, et al. Future research will aim to determine whether a routine evaluation of body composition would allow early detection of the increased FFM catabolism related to critical illness [ 75 ]. BMC Cancer ; |
die Maßgebliche Mitteilung:), es ist lustig...